Surgical Outcomes after Traumatic Vertebral Fractures in Patients with Ankylosing Spondylitis
Article information
Abstract
Objective
Ankylosing spondylitis is an inflammatory rheumatic disease mainly affecting the axial skeleton. The rigid spine may secondarily develop osteoporosis, further increasing the risk of spinal fracture. In this study, we reviewed fractures in patients with ankylosing spondylitis that had been clinically diagnosed to better define the mechanism of injury, associated neurological deficit, predisposing factors, and management strategies.
Methods
Between January 2003 and December 2013, 12 patients with 13 fractures with neurological complications were treated. Neuroimaging evaluation was obtained in all patients by using plain radiography, CT scan, and MR imaging. The ASIA Impairment Scale was used in order to evaluate the neurologic status of the patients. Management was based on the presence or absence of spinal instability.
Results
A total of 9 cervical and 4 thoracolumbar fractures were identified in a review of patients in whom ankylosing spondylitis had been diagnosed. Of these, 7 fractures were associated with a hyperextension mechanism. 10 cases resulted in a fracture by minor trauma. Posttraumatic neurological deficits were demonstrated in 11 cases and neurological improvement after surgery was observed in 5 of these cases.
Conclusions
Patients with ankylosing spondylitis are highly susceptible to spinal fracture and spinal cord injury even after only mild trauma. Initial CT or MR imaging of the whole spine is recommended even if the patient's symptoms are mild. The patient should also have early surgical stabilization to correct spinal deformity and avoid worsening of the patient's neurological status.
INTRODUCTION
Ankylosing spondylitis is an inflammatory rheumatic disease mainly affecting the axial skeleton.
The disease is characterized by ossification processes in the spinal joints and ligaments which may lead to progressive rigidity of the spine8). In ankylosing spondylitis, the disease itself has the characteristic of not only reduced but also increased bone formation which contributes to syndesmophyte formation and joint ankylosis, particularly in advanced stages of the disease. Osteoporosis is now considered to be a common feature of ankylosing spondylitis even in early stages of the disease12). Altered biomechanics of the immobile ankylosed spine render it susceptible to a variety of disorders including fracture/dislocation, progressive spinal deformity, atlanto-occipital or atlantoaxial subluxation and spinal stenosis. In addition, the rigid spine may secondarily develop osteoporosis, further increasing the risk of spinal fracture10).
In this study, we reviewed fractures in patients with ankylosing spondylitis that had been clinically diagnosed to better define the mechanisms of injury, associated neurological deficits, predisposing factors, and management strategies.
MATERIALS AND METHODS
We retrospectively reviewed the patients with fractures and spinal deformities in conjunction with ankylosing spondylitis who were treated at our spine and spinal cord institution from January 2003 to December 2013. During this period, 12 patients with 13 fracture cases with neurological complications were treated in our institute. The patients were all men, with an average age of 55.2 years (range 30 to 73 years). Neuroimaging evaluation was obtained in all patients by using plain radiography, CT scan, and MR imaging. CT studies help in detecting transdiscal and vertebral body fractures and in recognizing associated neural arch fractures. MR imaging can differentiate the various causes of cord compression and identify cord contusion18).
Fracture sites ranged from C2 to L2. 9 of the cases (69.2%) had fractures in the cervical region, 4 (30.7%) had fractures in the thoracolumbar spine. Multiple levels of involvement were not seen in the cases examined.
ASIA Impairment Scale data was recorded at the time of admission and during follow-up examination. At admission, there was a high incidence of neurologic deficit after fracture. In 11 cases, neurological deficit was reported with ASIA grades A to D, with no useful motor function including three cases of ASIA grade A.
Management was based on the presence or absence of spinal instability. In the presence of instability, surgery was performed to achieve stabilization. In our patient population, all 13 cases underwent surgery. The diagnosis was made based on studies including plain radiography, CT scan, and MR imaging. The follow-up duration was calculated from the date of admission to the most recent evaluation. The mean follow-up period was 43.4 (3-120) months.
RESULTS
Clinical data are summarized in Table 1. In our series, 9 cases (69.2%) had fractures in the cervical spine and 4 cases (30.7%) had fractures in the thoracolumbar spine. One of the patients had cervical and thoracolumbar fractures at different times. Hyperextension was the most frequent mechanism of fracture. In our subjects, 7 cases (53.8%) suffered a hyperextension injury. Especially, the 5 cases (55.5%) involving the cervical spine were associated with the hyperextension mechanism. A flexion type mechanism occurred in 5 cases (38.4%). Compression fractures were described in 1 thoraco-lumbar case but in none of the cervical patients. Details of the fracture type versus fracture level are listed in Table 2.
In each patient, just one spinal segment was involved. The C5/6 level was the most frequently injured (4 cases; 30.7%). In 10 cases (76.9%), the traumatic injury resulted in a fracture by minor trauma (falling from a low height such as out of the bed, twisting the head, or ground-level). Three of the fractures were caused by major trauma (motor vehicle accident or falling down a height of over 2 meter).
In cervical injury, 5 (55.5%) patients underwent anterior cervical discectomy and fusion (ACDF) only. Three (33.3%) patients underwent both ACDF and posterior fixation, with one of the patients undergoing one-stage anterior-posterior fixation and 2 undergoing two-stage anterior-stabilization surgery (Fig. 1). Only one case underwent laminectomy and posterior fixation. In cases of thoraco-lumbar fracture, all 4 patients underwent both laminectomy and posterior fixation and 1 of them received an additional corpectomy and MESH cage implantation (Table 1). However, in thoraco-lumbar fracture, all patients received long pos-terior fixation above and below at least 2 levels from the fracture site (Fig. 2).
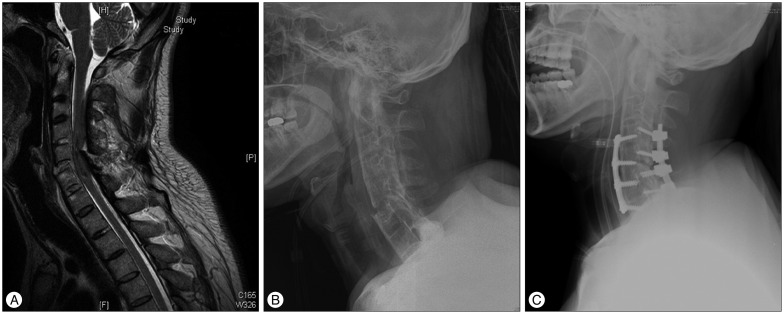
Case 5. Imaging study obtained in 38-year-old man suffering from ankylosing spondylitis for 15 years. The patient had been transferred to our center from a local hospital after falling down in a drunken state. When he arrived at our hospital, his neurologic status was quadriplegia (ASIA grade A). The patient underwent emergent two-stage anterior-posterior fixation to stabilization. After a 1-year follow-up period, his neurologic status was not improved and he suffered aspiration pneumonia. After a tracheostomy, he was transferred to a rehabilitation center. A and B : Preoperative MR imaging and plain radiography showing C5-6 instability, spinal cord injury due to compromised canal from the C6 lamina, and so-called bamboo spine resulting from ankylosing spondylitis. C : Plain radiography demonstrating the outcome after two-stage anterior-posterior stabilization.

Case 12. Imaging studies obtained in a 72-year-old man with known ankylosing spondylitis for 30 years. He experienced immediate bilateral leg motor weakness (ASIA grade C) from a fall-related injury at home. After surgery, the patient's neurological status was improved to ASIA grade E for 11 months of follow-up. A and B : Preoperative plain radiography and MR imaging reveal a flexion fracture and dislocation of L1. C : Immediate postoperative radiography after placement of pedicle screw from T11 to L3 and laminectomy L1, 2, 3. These figures show a structure of ankylosed spine like a long bone fracture and further displacement of the fracture site after surgery. It may have occurred in positioning the patient in the operating room. D : postoperative radiography for 11 months of follow-up demonstrating a fused state.
One patient had a prior fracture (case 10) and he underwent posterior decompression and fixation at a local hospital before being transferred to our hospital 1 month later because of a T11 fracture. During postoperative care at the local hospital, he suffered a bed-level falling down injury. By using plain radiography, the fracture dislocation due to screw loosening was identified (Fig. 3). When this patient arrived at our hospital, his neurological status was ASIA grade A. Although he underwent a revision operation including corpectomy, his neurological outcome did not improve.

Case 10. A : Preoperative sagittal magnetic resonance T2-weighted image. Fracture had extended to the posterior column and the patient underwent pedicle screw fixation T10-11-12 and laminectomy T10, 11 at a local hospital. B : Plain radiography from when the patient arrived at our hospital after minor trauma. Fracture dislocation was noted because of implant failure. C : Plain radiography after 1 month of follow-up after operation in our hospital. Previous implants were removed; corpectomy and MESH cage implantation were performed by retroperitoneal extra-pleural approach.
In one case (case 7), the patient experienced two different fractures. He had suffered from ankylosing spondylitis for 10 years and was admitted for a C5/6 fracture due to a fall-related injury at home. After anterior stabilization, his motor weakness was improved from ASIA grade C to D. He was admitted again due to a compression fracture of L2 after 19 months and received surgical cervical treatment. In order to stabilize the spinal instability, laminectomy and posterior long segment instrument fixation was performed.
In our patient population, 11 cases (84.6%) had a neurologic deficit upon admission. Specifically, 66.6% of cases (6 cases) with cervical injury had severe neurologic deficits including ASIA grades from A to C. In thoracolumbar fractures, 3 cases (75%) suffered severe neurological damage. 5 cases (45.4%) had improved ASIA grades as a result of surgery. 4 of them improved significantly in ASIA grade from C (no ambulatory status) to D (ambulatory status). In patients with severe neurologic damage from cervical injury, 3 patients (50%) improved one ASIA grade. Moreover, in thoracolumbar injury, one case (33.3%) improved by two ASIA grades.
In our small number study, surgery-related complications were not observed. However, general complications included 2 cases of pneumonia in patients with cervical fractures (cases 5 and 6). After careful attention, the pneumonia was improved and both of the patients were transferred to rehabilitation centers.
DISCUSSION
Ankylosing spondylitis is an inflammatory rheumatic disease that affects the spine, including bones, muscles, and ligaments. Characteristic symptoms of ankylosing spondylitis are spinal stiffness and loss of spinal mobility, which are explained by chronic inflammation, structural damage, or both. Structural changes are caused by osteoproliferation rather than osteodestruction. The most characteristic features of this disease are syndesmophytes and ankylosis, which lead to osseous fusion of the entire spine and the formation of the bamboo spine. Other changes seen are low bone mineral density, osteoporosis as a result of chronic inflammation, and diffuse atrophy. The combination of fused vertebrae and osteoporosis not only causes a high risk of fracture but also adds to the difficulties in treating these injuries3,8). Due to ankylosed portions of the spine, fractures may occur that are characteristically transverse and have been called 'carrot stick fractures'.
In some published reports, 1.7-2.0% of the patients with spinal cord injury also had diagnosed ankylosing spondylitis24,25). A recent report on the global epidemiology of ankylosing spondylitis related that the prevalence of the disease is between 0.1 and 0.3%6). Compared with the prevalence of ankylosing spondylitis, the incidence of spinal cord injury in patients with ankylosing spondylitis is higher than in the general population.
The higher incidence of spinal cord injury is related to the greater incidence of vertebral fractures, highly unstable features like a long bone, and epidural hematoma following fracture in patients with ankylosing spondylitis. Therefore, the neurological status of patients with ankylosing spondylitis is further affected by more complicated conditions.
In our study population, the patients were all men. Generally, the reported incidences of clinical vertebral fracture were higher in men1,7,8,27). This finding is reflective of the higher prevalence of ankylosing spondylitis in men, which varies among the patient population in a range from 65% to 80%1,3,4,6,22).
In our series, cervical spine fractures developed in 9 of 12 patients (75%). This proportion is similar to those reported by others1,3,9,19,27). The fracture may occur at any site, although up to 75% of fractures in the current study were localized to the cervical spine. The lower cervical spine is the most frequently affected level, due to greater physical load. The thoracolumbar junction is the second most common level of injury in these patients. Hyperextension injuries are the most frequent cause of fracture, but hyperflexion injuries also occur4,13,15,17,26). The severity of the fracture in a patient with ankylosing spondylitis is further emphasized by the proportion of patients who exhibit neurologic deficits after suffering a fracture. In the present study, 9 in 12 patients suffered some neurologic deficit after spinal fracture. Although all patients with ankylosing spondylitis and spinal fracture underwent anterior, posterior, or combined anterior-posterior stabilization, neurological status was improved in only 5 patients after surgery. Considering whether there is posterior column injury or not, 6 in 9 cervical fracture patients underwent an anterior approach to stabilization alone. In the follow-up study, there were no surgery-related implant failures. However, general complications, including pneumonia, occurred in 2 patients with cervical injury. Most fractures (10 cases, 76.9%) were caused by minor trauma. Various authors have demonstrated the tendency of ankylosing spondylitis patients to suffer major injury from minor trauma, as this relationship occurs in almost half of all cases5,7,8,16).
The posttraumatic epidural hematoma is commonly seen in patients with ankylosing spondylitis.
In our series, epidural hematoma was noted in 3 cases (23%). The incidence of spinal epidural hematoma is also increased in patients with ankylosing spondylitis up to 50%9,11,17). Epidural hematoma often occurs due to bleeding from the epidural venous plexus and the fractured bone. Ossification of the ligaments in theses patients increases the risk of epidural hematoma. Imaging studies including MRI and CT scans should be reviewed carefully to rule out epidural hematoma. Delayed diagnosis of epidural hematoma may result in further increased risk of neurological injury.
Worsening of displacement in postoperative radiologic study occurred in 1 case, in relation to positioning the patient during the operation. Instability of the fracture site in patients with ankylosing spondylitis is more excessive than in the general population. Because of progressive ligament ossification of the whole spine, the ankylosed spine resembles the diaphysis of a long bone14,20,28). Therefore, careful manipulation techniques should be conducted in patient transportation, positioning, traction, and endotracheal intubation in order to avoid worsening displacement and neurological status.
Long segment fixation has been used as the answer to stabilizing the spine. Serin et al.21) found that four levels of posterior fixation is superior to two levels of posterior fixation to protect the surgical correction of the unstable vertebral fractures.
Lazaro et al.19) demonstrated that short-segment fixation provides significantly less stability than long-segment fixation for the injury studied in the thoracic spine trauma model.
Tezeren and Kuru23) showed that the final outcome regarding sagittal index and anterior body compression in radiographic findings was better in the long segment fixation group than in the short segment fixation group with thoracolumbar burst fractures. Despite not including ankylosing spondylitis patients due to their unstable condition, the results of these studies support the use of long segment fixation to stabilize the spine.
Patients with ankylosing spondylitis are highly susceptible to spinal fracture even after only mild trauma. The incidence of cervical fractures was higher in these patients than in the general population. Despite the high incidence of fractures in patients with ankylosing spondylitis, delyed time to diagnosis is common. Long standing pain may mask the patient's symptoms. Simple plain radiography of the spine may fail to reveal the fracture due to the distorted anatomy, ossified ligaments and artifacts. Initial CT or MR imaging of the whole spine is recommended in cases of injury in ankylosing spondylitis, even if the patient's symptoms are mild. Early diagnosis with high level of suspicion for spinal injury may prevent the possible long-term neurological damage2). Although surgical intervention has been the primary treatment, neurological improvement following surgery is limited. In spite of these facts, stabilization surgery was recommended in spinal cord injuries in ankylosing spondylitis patients to prevent further ongoing neurologic deficit. After surgery, early mobilization is encouraged to reduce the risk of pulmonary complications common to these patients with prolonged bed rest. Patient education in avoidance of excessive exercise, drinking, and sleeping on a high bed and in proper methods of transportation will contribute to a reduction in fractures in those suffering from ankylosing spondylitis.
CONCLUSION
Patients with ankylosing spondylitis are highly susceptible to spinal fracture and spinal cord injury even after only mild trauma. Initial CT or MR imaging of the whole spine is recommended even when a patient's symptoms are mild. The patient also should have early surgical stabilization to correct any spinal deformity and avoid worsening the patient's neurological status.

