Delayed Dural Arteriovenous Fistula after Microvascular Decompression for Hemifacial Spasm
Article information
Abstract
Dural arteriovenous fistula (AVF) is very rare, acquired lesion that may present with intracranial hemorrhage or neurological deficits. The etiology is not completely understood but dural AVF often has been associated with thrombosis of the involved dural sinuses. To our knowledge, this is the first well documented intracranial hemorrhage case caused by dural AVF following microvascular decompression for hemifacial spasm. A 49-year-old male patient had left microvascular decompression of anterior inferior cerebellar artery via retrosigmoid suboccipital craniotomy. The patient was in good condition without any residual spasm or surgery-related complications. However, after 10 months, he suffered sudden onset of amnesia and dysarthria. Computed tomography and magnetic resonance imaging revealed the presence of dural AVF around the left transverse-sigmoid sinus. The dural AVF was treated with Onyx® (ev3) embolization. At the one-year follow up visit, there were no evidence of recurrence and morbidity related to dural AVF and its treatment. This case confirms that the acquired etiology of dural AVF may be associated with retrosigmoid suboccipital craniotomy for hemifacial spasm, even though it is an extremely consequence of this procedure.
INTRODUCTION
Hemifacial spasm (HFS) is a relatively rare movement disorder most commonly caused by vascular compression of the facial cranial nerve at its root exit zone from the brainstem. It is characterized as involuntary intermittent twitching of the muscles of the face. Microvascular decompression (MVD) was initially introduced by Gardner and Sava6). and was popularized by Jannetta et al.9). Since its introduction as a treatment for HFS, MVD via retrosigmoid suboccipital approach has become the treatment of choice due to its excellent results and low operative complications. Potential complications following MVD include hearing deficit, facial palsy, cerebrospinal fluid (CSF) leakage, low cranial nerve palsy, hemorrhage, cerebellar injury, meningitis, and death12,17). The delayed post-operative dural arteriovenous fistula (AVF) is very rare complication of this approach and has rarely been reported to date. In this report we present a case of delayed postoperative dural AVF occurring at the surgical site after retrosigmoid suboccipital craniotomy for MVD in a patient with HFS.
CASE REPORT
A 49-year-old man, ten months prior to his present admission, had been operated in our institution for left HFS caused by vascular compression of the facial nerve by the left anterior inferior cerebellar artery (AICA) (Fig. 1). There were no evidence of pathologic lesions such as hemorrhage, sinus thrombus, vascular malformation, tumors in preoperative imaging studies, including computed tomography (CT) and magnetic resonance imaging (MRI). A left retrosigmoid suboccipital craniotomy was performed to alleviate the spasm. The size of the craniotomy was relatively small and about twice the size of a quarter coin. At the time of the operation, we did not expose the transverse and sigmoid sinuses of the patient. At the end of the operation, we performed a watertight dural closure. The muscle and scalp were closed in the anatomical layers. The patient's hemifacial spasm completely disappeared postoperatively. Ten months after the operation, the patient complained of amnesia and dysarthria. The patient had no history of head trauma before and after operation. CT showed intracranial hemorrhage (ICH) on left temporoparietal subcortical area (Fig. 2A) and CT angiography (CTA) showed the abnormal enhanced vessels on left transverse-sigmoid sinus (Fig. 2B). Magnetic resonance angiography (MRA) clearly showed a dural AVF at the site of the previous surgery (Fig. 2C, D). Digital subtraction angiography (DSA) demonstrated a dural AVF of the left transverse-sigmoid sinus fed by the left occipital artery (Fig. 3A). After superselective catheterization of the left occipital artery, which supplied the affected sinus of the dural AVF, embolization with Onyx® (total 3.5 cc; ev3, Irvine, CA, USA) was performed successfully (Fig. 3B). One year later, follow-up DSA did not showed any recurrence of lesion (Fig. 3C). The patient's condition was in normal without recurrence of hemifacial spasm.
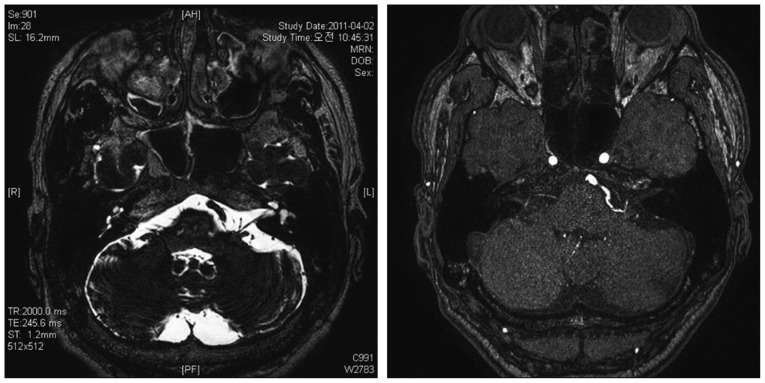
Preoperative magnetic resonance image show that left anterior inferior cerebellar artery compressed left facial nerve at the root exit zone.
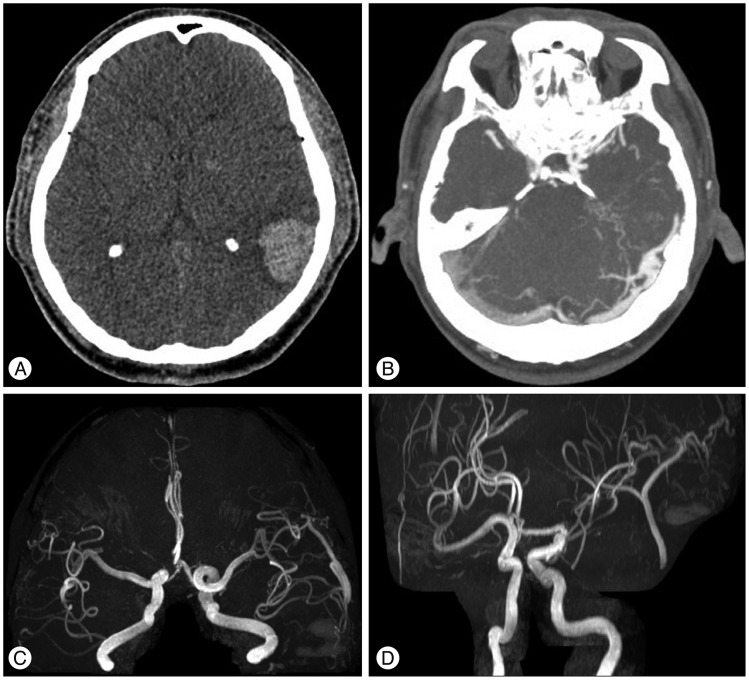
A : Computed tomography (CT) shows the high density lesion on the left temporoparietal subcortical area. B : CT angiography shows the abnormal enhanced vessels on left transverse-sigmoid sinus. C and D : MRAs show dural arteriovenous fistula that has occipital artery as a feeder and draining transverse-sigmoid sinus.
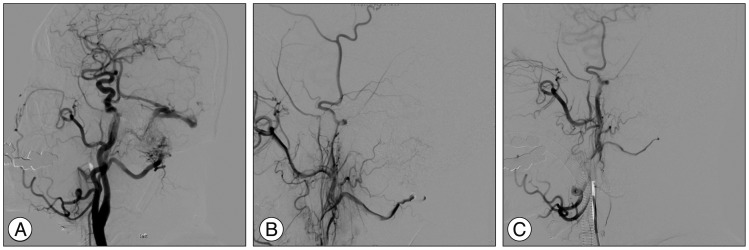
A : Pre-embolizational left external carotid artery angiographic image shows the dural AVF with feeders from left occipital artery. B : Post-embolizational angiographic image shows nearly complete occlusion of left sigmoid sinus dural arteriovenous fistula (AVF). C : There is no residual dural AVF at the follow-up angiography obtained 12 months after embolization.
DISCUSSION
Dural AVF is low pressure, spontaneously occurring communications between vessels of internal and external carotid origin that supply the dura and a dural venous sinus. Dural AVFs are relatively rare, with a prevalence of 0.15 per 100000 people per year, and constitute 6-15% of all intracranial AVFs with most being located in the posterior fossa2). Although the etiology of dural AVFs is still controversial, they are generally classified into congenital or acquired. Acquired dural AVFs have been reported to develop secondarily to sinus thrombosis8,19,21), head injury4), cerebral infarction7), and craniotomy18). Among the variable causes, acquired dural AVF after craniotomy had rarely been reported18,21,22). Although the time of occurrence, location, and type of surgery were variable according to the reports, sinus thrombosis, thrombophlebitis, and late intrasinus hypertension following sacrifice of the venous sinus were suggested as underlying mechanism of dural AVF19).
In our case, the dural AVF developed at the site of the previous craniotomy was not associated with sacrifice of the transverse-sigmoid sinus or trauma. Also, there were no evidence of dural sinus thrombosis in the preoperative imaging studies. There was one report which addressed the symptomatic dural AVF after craniotomy for the trigeminal neuralgia surgery18). Different from previous report, our case was unique in nature that the initial presentation of the AVF was intracranial hemorrhage, which was confirmed in the CT scan. Maybe our case is the first report in which the dural AVF after craniotomy was initially presented as ICH. Besides, this initial presentation of dural AVF would lead to difficulties in exact diagnosis. At this point, CTA and MRA was very effective tool which confirmed the dural AVF as a cause of ICH.
The first option of treatment for dural AVF is transarterial embolization1,10). Although the coil embolization is an attractive option, transarterial Onyx® embolization has recently been recommended as a safe therapeutic alternative. It is very effective with type I and II dural AVF through the Cognard classification because it reduces the shunted blood flow and facilitates subsequent transvenous embolization or surgery. However, Onyx® embolizations15) have limitations and risks, including cardiac Onyx® embolization5), reflexive bradyarrhythmia16,20), visual hallucination, and cranial nerve palsy3). If the transarterial or transvenous embolization failed, we considered the next treatment option to be surgical interruption of the fistulas13,21) or radiosurgery11,14). In our case, the dural AVF was completely obstructed during initial procedure and there were no leakage or evidence of complication in the immediate and late (12 months) follow-up angiography. Therefore, no further surgeries were needed and the patient was benefitted from this minimally-invasive procedure.
CONCLUSION
The dural AVF is rare complication after retrosigmoid suboccipital craniotomy and intensive monitoring for the complication would be warranted after microvascular decompression.