Comparative Analysis of Endovascular Stroke Therapy Using Urokinase, Penumbra System and Retrievable (Solitare) Stent
Article information
Abstract
Background
Higher reperfusion rates have been established with endovascular treatment for acute ischemic stroke patients. There are limited data on the comparative performance of mechanical thrombectomy devices. This study aimed to analyse the efficacy and safety of the stent retriever device (Solitaire stent) by comparing procedure time, angiographic outcome, complication rate and long term clinical outcome with previous chemical thrombolysis and mechanical thrombectomy using penumbra system.
Methods
A retrospective single-center analysis was undertaken of all consecutive patients who underwent chemical thrombolysis and mechanical thrombectomy using Penumbra or Solitaire stent retriever from March 2009 to March 2014. Baseline characteristics, rate of successful recanalization (modified Thrombolysis in Cerebral Infarction score 2b-3), symptomatic intracerebral hemorrhage, procedure time, mortality and independent functional outcomes (mRS ≤2) at 3 month were compared across the three method.
Results
Our cohort included 164 patients, mechanical thrombectomy using stent retriever device had a significant impact on recanalization rate and functional independence at 3 months. In unadjusted analysis mechanical thrombectomy using Solitaire stent retriever showed higher recanalization rate than Penumbra system and chemical thrombolysis (75% vs. 64.2% vs. 49.4%, p=0.03) and higher rate of functional independence at 3 month (53.1% vs. 37.7% vs. 35.4%, p=0.213). In view of the interrelationships between all predictors of variables associated with a good clinical outcome, when the chemical thrombolysis was used as a reference, in multiple logistic regression analysis, the use of Solitaire stent retriever showed higher odds of independent functional outcome [odds ratio (OR) 2.62, 95% confidence interval (CI) 0.96-7.17; p=0.061] in comparison with penumbra system (OR 1.57, 95% CI 0.63-3.90; p=0.331).
Conclusion
Our initial data suggest that mechanical thrombectomy using stent retriever is superior to the mechanical thrombectomy using penumbra system and conventional chemical thrombolysis in achieving higher rates of reperfusion and better outcomes. Randomized clinical trials are needed to establish the actual benefit to specific patient populations.
INTRODUCTION
Proximal intracranial artery occlusion is one of the most common cause of acute ischemic stroke which can carry a particularly high burden of long-term disability and mortality318). And recanalization of occluded large vessel is proven to be an important factor for favorable outcome in acute ischemic stroke4).
Since intravenous recombinant tissue plasminogen activator emerged in 1996 as the first United States Federal Food and Drug Administration (FDA) approved treatment for acute ischemic stroke (AIS), the treatment for acute ischemic stroke evolved to include intravenous thrombolysis until 4.5 hrs after onset121). However, there were still some limitations in intravenous (IV) thrombolysis, such as the narrow therapeutic time window and low reperfusion rate in the proximal segment of the large intracerebral artery. To overcome these limitations, endovascular treatment for acute ischemic stroke, including intra-arterial (IA) chemical thrombolysis and mechanical thrombectomy were introduced, and has been developed during last decades with offering an expanded time window 6 to 8 hours1172021).
Mechanical thrombectomy was initially introduced as a complementary treatment to AIS therapy, particularly when IV or IA chemical thrombolysis is ineffectual. In 2004, the Merci Retriever (Stryker Neurovascular, Mountain View, CA, USA) became the first FDA approved mechanical thrombectomy device in the treatment of AIS, Since then, there has been an explosive of interest into mechanical thrombectomy devices and many new devices have been developed. The newer generation mechanical thrombectomy devices such as Penumbra Aspiration System (Penumbra, Alameda, CA, USA) and Stent Retriever (Solitaire; ev3, Irvine, CA, USA) showed that these devices are significantly better at restoring blood flow in occluded arteries compared with the Merci Retriever121619).
This study aimed to analysis the efficacy and safety of the stent retriever device (Solitaire stent) by comparing procedure time, angiographic outcome, complication rate and long term clinical outcome between previous chemical thrombolysis and mechanical thrombectomy using penumbra system.
MATERIALS AND METHODS
Data collection
We retrospectively reviewed clinical and imaging data of patients with acute cerebral infarction who treated with endovascular procedure (mechanical thrombectomy using Solitaire stent retriever device or Penumbra system and chemical thrombolysis) at our institution over 5-year period (March 2009 to March 2014). The law data were obtained from stroke registry data which collected prospectively and retrospective image analysis was done through the hospital's Picture Archive and Communication System system.
Patients
Patients were eligible if they presented within 8 hours of symptom onset with a baseline National Institutes of Health Strike Scale (NIHSS) score of ≥8 and angiographically confirmed a proximal (the first and second segment) middle cerebral artery occlusion and distal intracerebral artery occlusion.
Eligible patients that met the standard National Institute of Neurological Disorder and Stroke criteria for intravenous recombinant tissue plasminogen activator (rt-PA) were initially treated with intravenous thrombolysis and subsequent endovascular therapy was considered refractory to intravenous thrombolysis. Patients with extensive infarctions greater than one third of territory of the middle cerebral artery (MCA), severe edema, and intracerebral hemorrhage (ICH) were excluded.
Patients who had acute cerebral infarctions caused by occlusion of the distal common carotid artery, proximal ICA, and vertebrobasilar circulation were excluded for suggestion of unified clinical inclusion criteria and result analysis. Patients who treated by multiple devices for rescue treatment was also excluded for calculating pure treatment results of each treatment method.
Data sources/measurement
In our retrospective analysis, the collected patients data were age, sex, risk factor, Trial of Org 10172 in Acute Stroke Treatment classification, NIHSS on admission and at discharge (baseline NIHSS), use if IV rt-PA, duration of the procedure (symptom onset to puncture time and puncture to recanalization time), presence of symptomatic hemorrhage, final recanalization status, NIHSS at discharge, and clinical functional outcome at 3 months. Successful recanalization was defined as modified Thrombolysis In Cerebral Ischemia (mTICI) grades 2b to 3. Symptomatic hemorrhage was defined by (according to) the Safe Implementation of Thrombolysis in Stroke Monitoring Study criteria; local or remote parenchymal hemorrhage on the imaging can obtained at 24 h that caused a mass effect, with clinical deterioration as indicated by a score on the NIHSS that was higher by ≥4 points than the baseline value. Clinical functional outcome was assessed with the modified Rankin Scale (mRS) by a stroke neurologist, at discharge and 3 month after treatment. Favorable clinical outcome was defined as mRS score of ≤2.
Procedure
All endovascular therapies were performed on a biplane angiography machine (Siemens Axiom Artis, Siemens Healthcare, Erlangen, Germany), cerebral angiography and endovascular therapy were performed under local anesthesia. In case of agitation, IV bolus of midazolam or thiopental was given and repeated. After target vessel was verified angiographically and rated on the mTICI scale, 6 Fr standard guiding catheter (Envoy, Cordis Corporation International, Johnson and Johnson Medical NV/SA, Waterloo, Belgium) was placed in the petrous or cervical portion of ICA. The guiding catheter was continuously flushed with heparinized saline. A balloon guiding catheter was not used in any patients.
Chemical thrombolysis
Chemical thrombolysis was performed aggressive mechanical catheterization using microcatheter and J-shaped guide-wire tip within the clot. A microcatheter was navigated with a 0.021-microcatheter middle portion of the clot, aggressive mechanical clot disruption using microcatheter was performed with injecting urokinase until a Thrombolysis In Cerebral Infarction grade of ≥2b was reached. If IV rt-PA was administered, the amount of urokinase that is used is up to 800000 IU, but if it is not administered, it was up to 1000000 IU.
Mechanical thrombectomy
Penumbra system
Mechanical thrombectomy using Penumbra system, forced arterial suction thrombectomy with a Penumbra reperfusion catheter was performed. An appropriate guide catheter was brought into the position in the occluded target vessel, reperfusion catheter was navigated proximal to the clot. The appropriate position was achieved proximal to the clot, the guidewire was removed from the Penumbra reperfusion catheter. Reduction of the clot burden by aspiration was accomplished by connecting 50 cc syringe pump under continuous aspiration into the guiding catheter with 50 cc syringe. When the subsequent control angiography showed a TICI grade <2, clot aspiration with the reperfusion catheter was reattempted until a TICI grade of ≥2b was reached (Fig. 1).

A : Pretreatment angiography shows complete occlusion of the M1 segment of the left MCA. B : A Penumbra 041 reperfusion catheter was approached proximal to the thrombus, and aspiration thrombectomy maneuver was performed. C : Immediate postprocedural angiography shows complete (TICI 3) revascularization. D : Photograph shows that whole clot retrieved from the occlusion of the left MCA. TICI : Thrombolysis In Cerebral Ischemia, MCA : middle cerebral artery.
Stentriever (Solitaire)
The target vessel was navigated with microcatheter (Rebar, ev3) distal to the clot over a microwire. The Solitaire stent, which was 4 mm in diameter and 20 mm long or 6 mm in diameter and 30 mm long was then introduced through the microcatheter and fully deployed across the occluded segment. A control angiography was performed after successful deployment of the stent device to evaluate re-establishment of flow. After the stent was maintained in place for 3 min, the fully deployed stent and the delivery microcatheter were pulled back together under continuous aspiration into the guiding catheter with 50 cc syringe. After removal of the stent and microcatheter, another 20 cc of blood was aspirated from the guiding catheter to prevent distal migration of possibly lost clot. When the subsequent control angiography showed a TICI grade <2, clot retrieval with the Solitaire stent was reattempted until a TICI grade of ≥2b was reached or until three passes (Fig. 2).

A : Pretreatment angiography shows complete occlusion of the M1 segment of the right MCA. B : Digital subtraction angiogram after deployment of the stent shows reopening of the vessel. C : After stent withdrawal, the vessel is fully recanalized. D : Photograph of gross analysis of the Solitaire device (ev3, Irvine, CA, USA) showing clot fragments within the stent retrieval system. MCA : middle cerebral artery.
Statistical analysis
SAS (version 9.3, SAS Institute, Cary, NC, USA) software was used to perform the statistical analysis. Analysis of variance (ANOVA) and median test was performed to compare each normally and non-normally distributed continuous variable among the treatment methods. The chi-square homogeneity test was used to compare categorical variables. Binary logistic regression was conducted for successful recanalization and favorable functional outcome mRS at 3 months. In the logistic regression for each effect of treatment methods evaluated. The significance level was set at below 5% for all statistics.
RESULTS
Patients enrolment
Between March 2009 and March 2014, a total of 259 consecutive patients with acute ischemic stroke were treated with endovascular recanalization method, among them 203 patients were caused by proximal middle large artery or distal internal carotid artery occlusion (56 patients caused by vertebrobasilar artery or proximal common carotid artery occlusion were excluded). Of these, 39 patients were excluded (13 underwent intracranial stenting, 16 underwent mechanical thrombectomy using multiple devices for rescue treatment, 10 did not require any further endovascular treatment due to spontaneous recanalization). Finally, 164 patients [32 patients (19.5%) treated with Solitaire stent retriever, 53 patients (32.3%) treated with Penumbra system, and 79 patients (48.2%) treated with chemical thrombolysis] were enrolled in this study.
Baseline characteristics
The mean age was 65±10.67 years, median NIHSS score (IQR) was 14.0 (11.0-17.0) and there were 94 (57.3%) men and 70 (42.7%) women. The site of occlusions included the middle cerebral artery (MCA) in 116 patients (70.7%) and the internal carotid artery terminus (T-occlusion) in 48 patients (29.3%). 73 patients (44.5%) were treated with IV rt-PA before the endovascular treatment.
The baseline characteristics were similar in the three groups except for a trend towards a higher predominance of T-occlusion [Solitaire retriever, n=8 (25%) vs. Penumbra system, n=25 (47.2%) vs. chemical thrombolysis, n=15 (19%); p=0.002] in the Penumbra system group (Table 1).
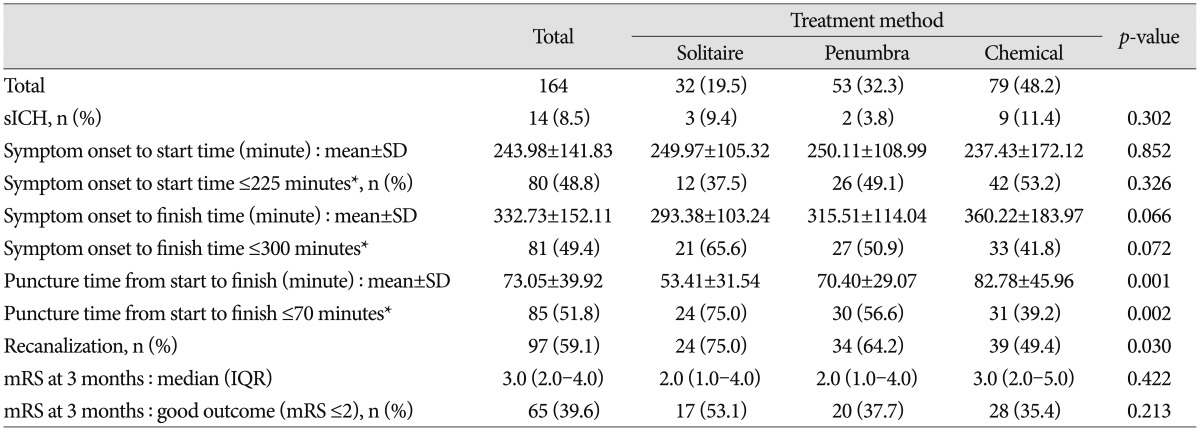
Clinical and radiologic outcomes
Table 2 summarize the unadjusted results of clinical, angiographic, and radiologic differences among the three groups. In the recanalization outcomes, mechanical thrombectomy using Solitaire stent retriever group showed highest rate of successful recanalization [Solitaire retriever, n=24/32 (75%) vs. Penumbra system, n=34/53 (64.2%) vs. chemical thrombolysis, n=39/79 (49.4%); p=0.030]. The mean procedure time (puncture to recanalization time) was also fastest in the Solitaire retriever group (Solitaire retriever, 53.41±31.54 min vs. Penumbra system, 70.40±29.07 min vs. chemical thrombolysis, 82.78±45.96 min; p=0.001), and all of the patients treated by Solitaire retriever recanalized within 70 minutes. So, though symptom onset to puncture time was fastest in the chemical thrombolysis group, the final symptom onset to recanalization time was fastest in the Solitaire stent retriever group (Solitaire retriever, 298.38±103.24 min vs. Penumbra system, 315.51±114.04 min vs. chemical thrombolysis, 360.22±183.97 min; p=0.066). The rates of symptomatic intracranial hemorrhage were not different among three groups (Solitaire retriever, n=3/32 (9.4%) vs. Penumbra system, n=2/53 (3.8%) vs. chemical thrombolysis, n=9/79 (11.4%); p=0.302).
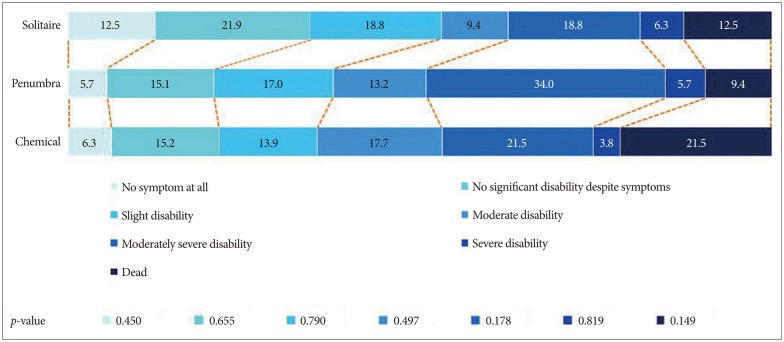
In the clinical outcomes, the mortality rate at 3 months were higher in the chemical thrombolysis group than Solitaire retriever and Penumbra group (Solitaire retriever, 12.5% vs. Penumbra system, 9.4% vs. chemical thrombolysis, 21.5%; p=0.030), and there was a trend towards better functional outcomes in Solitaire retriever group than Penumbra and chemical thrombolysis group (3 Mo mRS 0-2 : Solitaire retriever, 53.1% vs. Penumbra system, 37.7% vs. chemical thrombolysis, 35.4%; p=0.213) (Fig. 3).
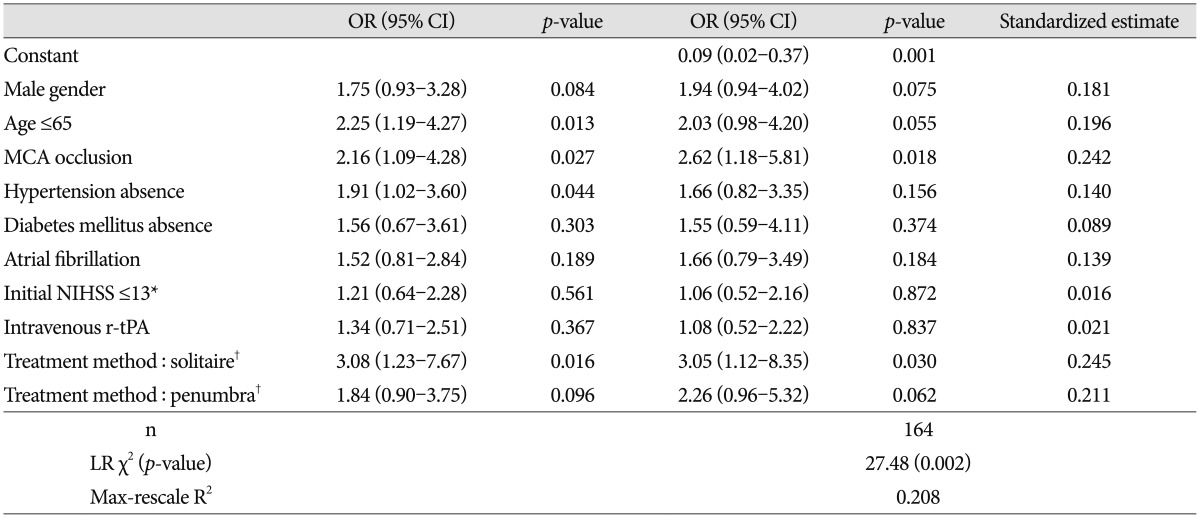
Logistic probability model for recanalization and favorable clinical outcomes
In the relationship between all predictors of variables associated with a successful recanalization and favorable clinical outcome, multiple logistic regression analysis was used. Successful recanalization was achieved more often in the Solitaire retriever group and Penumbra group than chemical thrombolysis group. In Multivariable analysis, when the chemical thrombolysis group was used as a reference, the use of Solitaire retriever was found to be a significant predictor of successful recanalization (OR 3.05, 95% CI 1.12-8.35; p=0.030), and Penumbra group showed an approached significance (OR 2.26, 95% CI 0.96-5.32; p=0.062) (Table 3). In the analysis of predictors affecting favorable clinical outcomes, excluded the procedure times and the reperfusion rates because of their colinear relationship with the treatment method used. The binary logistic model showed the following independent predictors of favorable clinical outcomes at 3 months : occlusion site (OR 5.77, 95% CI 2.19-15.15; p=0.004), absence of hypertension (OR 3.11, 95% CI 1.41-6.85; p=0.005), baseline NIHSS (OR 2.71, 95% CI 1.25-5.87; p=0.012), and mechanical thrombectomy using Solitaire stent retriever. When the chemical thrombolysis group was used as a reference, the use of Solitaire retriever showed an approached significance of favorable clinical outcomes (OR 2.62, 95% CI 0.96-7.17; p=0.061), whereas the Penumbra group outcomes showed comparatively higher odds but were statistically insignificant (OR 1.57, 95% CI 0.63-3.90; p=0.331) (Table 4).
DISCUSSION
Intravenous tissue plasminogen activator (IV t-PA) within 4.5 h of stroke onset is an effective treatment for acute ischemic stroke610). But it has still limitation of low recanalization rate when the occlusion site is in the proximal segment and narrow therapeutic window915). To overcome these limitations, endovascular treatment (EVT), including chemical thrombolysis and various mechanical thrombectomy within 6-8 h of symptom onset, has been introduced711). The last 10 years have seen major developments in the endovascular devices for removing clot in acute ischemic stroke.
Due to the first generation mechanical thombectomy devices such as Merci thrombectomy showed modest technical efficacy, the evolution of endovascular therapy to improve both efficacy and safety has been continued, the paradigm of treatment of acute ischemic stroke has shifted toward the newer generation mechanical thrombectomy devices including Penumbra system and stent retriever technique2121622).
The Penumbra Stroke Trial (multicenter, prospective, single-arm trial) reported the safety and efficacy of the device with the goal of establishing substantial equivalence to the Merci clot retrieval system. Although the recanalization rate was obtained in 81.6% of the cases (compared with 55% in the Multi-MERCI trial and 66% in the PROACT II trial), the neurological outcome was comparable or lower (25% with mRS ≤2, vs. 36% in the Multi-MERCI trial and 40% in the PROACT II trial).
The investigators attribute this disparity to the lack of sufficient power and higher baseline NIHSS score, high rate of symptomatic hemorrhage (11.2%) and overall mortality (32.8%) might explain this disparity high rate of successful recanalization with low rate of favorable functional outcome14).
Retrievable stents, known as stentrievers, unlike prior devices, facilitate the immediate restoration of blood flow via deployment of a stent within the clot. The stent integration into the clot also allows for subsequent clot and stent extraction, without any need for permanent device implantation.
Recently, the FDA granted clearance to both the Solitaire flow restoration stentriever device (ev3/Covidien Vascular Therapies, Irvine, CA, USA) and the Trevo Pro Retrieval System (Stryker) under 510 (k) clearance and 2 randomized clinical trials (Solitaire With the Intention For Thrombectomy and Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke) have compared newer clot retrieval devices with the Merci retriever in the treatment of acute ischemic stroke1216).
However, those studies obtained clinical and imaging data of stent assisted thrombectomy without comparing stent assisted thrombectomy with previous intra-arterial recanalization techniques such as conventional intra-arterial chemical thrombolysis or other contemporary mechanical thrombectomy technique such as Penumbra thrombectomy device.
The present study evaluated the technical safety and clinical benefit of stent assisted thrombectomy by comparing intra-arterial chemical thrombolysis and Penumbra thrombectomy.
The intra-arterial chemical thrombolysis group showed 49.4% successful recanalization rate and 35.4% favorable functional outcomes. It was difficult to compare that of previous studies as different scale were used, but when the criteria of successful recanalization was TICI ≥2a, our result showed 69.2% successful recanalization rate. It was comparable to the 63% recanalization rate of Thrombolysis in Myocardial Infarct (TIMI) ≥2 showed Prolyse in Acute Cerebral ThromboembolismII (PROACT II) study5) and 73.7% of partial or complete recanalization rate showed in the Middle Cerebral Artery Embolism Local Fibrinolytic Intervention Trial (MELT)13).
But the favorable functional outcome rate of our study was less than previous studies, the frequency of favorable functional outcome was 35.4% in our study, 40% in PROACT II, and 49.1% in MELT. Because of the different patients characteristics, which resulted from different inclusion criteria, complicate this indirect comparison.
The mechanical thrombectomy group using Penumbra aspiration showed 64.2% recanalization rate and 37.7% favorable functional outcomes. The thromboaspiration with Penumbra system showed less successful recanalization rate and favorable functional outcome rate compare to previous study of forced suction thrombectomy using the Penumbra reperfusion catheter which could achieve 81.9% successful recanalization rate with 45.5% favorable functional outcomes8).
It was also difficult to compare directly because of different patients characteristics such as higher proportion of T-occlusion in our study than previous study (47.2% vs. 18%) and different inclusion criteria.
In agreement with previously published SWIFT study, mechanical thrombectomy using Solitaire stentretriever showed high rate of successful recanalization with favorable functional outcomes. The mechanical thrombectomy using Solitaire stent retriever group showed 75% successful recanalization rate and 53.1% favorable functional outcomes at 3 months. It was comparable to the 69% successful recanalization rate with a TIMI flow ≥2 (assessed by core laboratory) and 58% favorable functional outcomes of SWIFT study.
Our data demonstrate that mechanical thrombectomy using stent retriever or Penumbra aspiration technique is more effective than chemical thrombolysis in terms of reperfusion rate and favorable clinical outcomes. And also suggest that thrombectomy using stent retriever is superior to the Penumbra thromboaspiration technique.
In multivariate analysis, when the chemical thrombolysis was used as a reference, the use of Solitaire stent retriever showed higher odds of favorable functional outcomes at 3 months than Penumbra thromboaspiration (2.62 vs. 1.57) (Table 4).
Although the reason for this discrepancy are uncertain, there are some possible explanation. Higher recanalization rates with short time intervals to recanalization have been suggested to be important to achieving favorable clinical outcomes. In our study, the use of Solitaire stent retriever was associated with higher rate of successful recanalization (75.0% vs. 64.2%). And when adjusted differences in clinical and radiological characteristics, the use of Solitaire stent retriever also showed higher odds of successful recanalization than Penumbra thromboaspiration (3.05 vs. 2.26) (Table 3).
The mean procedural times of successfully recanalized patients was shorter in the Solitaire stent retriever group than in the Penumbra thromboaspiration group (51.25 min Solitaire retriever vs. 70.41 min Penumbra aspiration), although there were no significant difference in the symptom onset to procedure start time between Solitaire stent retriever group and Penumbra aspiration group, the final time from symptom onset to recanalization was significantly shorter in the Solitaire stent retriever group than Penumbra aspiration group (293.38 min Solitaire retriever vs. 315.51 min Penumbra aspiration) (Table 2).
In conclusion, our study demonstrated in a multivariate analysis that the mechanical thrombectomy using Solitaire stent retriever showed highest rate of successful recanalization with shortest procedural time comparing with the mechanical thrombectomy using Penumbra thromboaspiration and chemical thrombolysis. And the use of Solitaire stent retriever in the mechanical thrombectomy of acute ischemic stroke could potentially be an independent predictor of favorable functional outcome at 3 months.
Our study have some limitations that included the data being collected retrospectively without randomized allocation and relatively small sample size. There were imbalances in the baseline characteristics among three groups. However, this study analyzed the prospective registry of consecutive patients and to overcome the imbalance of baseline characteristics, we performed a multivariate analysis adjusting for the difference. Furthermore, the single-center nature of our analysis, just only two operators performing all procedure, allowed for a more homogeneous approach to compare the different methods of endovascular recanalization.
Endovascular treatment is widely used as a reperfusion therapy. Nowdays, both technical expertise and technology evolve overtime. It is possible that more recent mechanical thrombectomy results would be superior. This analysis did not incorporate the result of newer Penumbra aspiration system, 5 MAX and the other stent retriever Trevo stent retriever because they were not commercially available during the duration of our study.
CONCLUSION
This study demonstrated that the mechanical thrombectomy using Solitaire retriever is superior to Penumbra thromboaspiration system and chemical thrombolysis and also the clinical implication of higher rate of favorable functional outcome with mechanical thrombectomy using Solitaire stent retriever. However, more evidence is needed such as randomized clinical trial comparing these endovascular recanalization techniques.
Acknowledgements
This work was supported by the Dong-A University Research Fund.