Recent Advancements of Treatment for Leptomeningeal Carcinomatosis
Article information
Abstract
Treatment of Leptomeningeal carcinomatosis (LMC) from solid cancers has not advanced noticeably since the introduction of intra-cerebrospinal fluid (CSF) chemotherapy in the 1970's. The marginal survival benefit and difficulty of intrathecal chemotherapy injection has hindered its wide spread use. Even after the introduction of intraventricular chemotherapy with Ommaya reservoir, frequent development of CSF flow disturbance, manifested as increased intracranial pressure (ICP), made injected drug to be distributed unevenly and thus, the therapy became ineffective. Systemic chemotherapy for LMC has been limited as effective CSF concentration can hardly be achieved except high dose methotrexate (MTX) intravenous administration. However, the introduction of small molecular weight target inhibitors for primary cancer treatment has changed the old concept of 'blood-brain barrier' as the ultimate barrier to systemically administered drugs. Conventional oral administration achieves an effective concentration at the nanomolar level. Furthermore, many studies report that a combined treatment of target inhibitor and intra-CSF chemotherapy significantly prolongs patient survival. Ventriculolumbar perfusion (VLP) chemotherapy has sought to increase drug delivery to the subarachnoid CSF space even in patients with disturbed CSF flow. Recently authors performed phase 1 and 2 clinical trial of VLP chemotherapy with MTX, and 3/4th of patients with increased ICP got controlled ICP and the survival was prolonged. Further trials are required with newly available drugs for CSF chemotherapy. Additionally, new LMC biologic/pharmacodynamic markers for early diagnosis and monitoring of the treatment response are to be identified with the help of advanced molecular biology techniques.
INTRODUCTION
Leptomeningeal carcinomatosis (LMC) is a dismal terminal stage disease of solid cancer that is devastating to the patient. Overall survival (OS) of patients with LMC is approximately 6-8 weeks, and intra-cerebrospinal fluid(CSF) chemotherapy show a survival benefit ranging from 3-9 months according to clinical variables153466).
Problems of intra-CSF chemotherapy include marginal survival benefit over systemic chemotherapy, difficulty of repeated drug injection, poor symptom improvement, and the occurrence of rare but serious side effects such as encephalopathy121319). Among these, CSF flow disturbance, manifest as increased intracranial pressure (ICP) and/or hydrocephalus, is not only a poor prognostic factor but also one of the reasons for treatment failure as it prevents even distribution of injected drugs within the CSF space183237). Research from the 1990s report that CSF flow disturbance is found in 40-60% of patients with LMC based on radionuclide cisternography2132). Once-disrupted CSF flow hardly recovers and increases the risk of encephalopathy via transependymal drug concentration gradient. Most patients quit chemotherapy to selectively receive a ventriculo-peritoneal shunt11618). Reported clinical studies are mainly retrospective, with a small number of patients, limited number of drug injection, and heterogeneous primary cancers. It is therefore difficult to draw any decisive conclusion about the effectiveness of intra-CSF chemotherapy.233850516566).
Chemotherapy for LMC is not curative but palliative. However, studies reporting the response of LMC-related symptoms are rare and the criteria for improvement are subjective385054). Some studies suggested that CSF profiles can be prognostic indicators, but show inconsistent findings of CSF profile change as a treatment response14233766). Another difficulty in evaluating the LMC treatment response is both, the inconsistency of CSF cytology and lack of quantitative measurement of the disease2566). Chamberlain and Kormanik17) suggest a criteria for CSF cytology response of 'two consecutive negative finding at least 1 week apart and sustained for 1 month' but fail to correlate patient survival and reach a general consensus.
It is difficult to estimate the number of clinicians and the frequency at which they apply intra-CSF chemotherapy in patients with poor prognosis, systemic cancer burden, and poor performance profiles. Patients need surgery for subcutaneous intraventricular reservoir for stable drug injection, and require evaluation of physiologic CSF flow and monitoring of drug concentration to avoid toxicities. Despite these difficulties, more aggressive intra-CSF chemotherapy prolongs patient survival in studies of one primary cancer with multiple drug injection and/or salvage intra-CSF chemotherapy172334).
Recently, there are two new trials in the treatment of LMC from solid cancer. First is the increasing application of receptor tyrosine kinase inhibitor (RTKi) for primary cancers, such as epidermal growth factor receptor (EGFR) inhibitor and HER-2 monoclonal antibody in addition to conventional intra-CSF chemotherapy. Prolonged survival is clinically observed in patients who receive RTKi concomitant with intra-CSF chemotherapy. The second is clinical trial of ventriculolumbar perfusion (VLP)3536). VLP is expected to circumvent ineffective drug delivery in LMC patients with disturbed CSF flow but was halted due to technical complexities2449). Authors successfully finished VLP phase 1 with pharmacokinetic data and the following phase 2 trial proved the effectiveness of VLP in LMC patients with increased ICP and prolonged patient survival3536).
RESULTS OF LMC TREATMENTS OVER THE DECADES
Treatment modalities for LMC
Treatments for LMC should cover the whole-neuraxis as the disease spreads. In this context, even whole brain radiation therapy (WBRT) is not an appropriate therapeutic modality for LMC, as it does not cover the entire CSF space and besides, cancer cells move along with the CSF flow. Recent retrospective study on 125 non-small cell lung cancer (NSCLC) patients with LMC demonstrates a lack of effectiveness of WBRT on patient survival48). Seven of these patients with intrathecal chemotherapy show significantly prolonged survival.
Meanwhile, either systemic or intrathecal chemotherapy achieves even distribution of drugs throughout the neuraxis. Pharmacokinetic studies with animal models done in the 1970's have predicted CSF levels of methotrexate (MTX) with clearance rate i.e., 3-5% of systemically administered MTX penetrates the blood-brain barrier (BBB) at a half-clearance time of 6 hours. Thus, to achieve a therapeutic concentration (>1 µM) of MTX in the CSF, grams of MTX are required to be administered intravenously for days5561). Single intraventricular injection of MTX (6.25 mg/m2) can achieve therapeutic concentration in the lumbar space for 48 hours at a minimal systemic absorption (<0.1 µM). Additionally, use of intraventricular Ommaya reservoir has the advantage of patient comfort especially in repeated frequent injection, prevention of drug leakage, and better drug distribution as compared to the intrathecal (via lumbar puncture) chemotherapy59). Thus, studies with repeated aggressive intra-CSF chemotherapy mostly adopt the Ommaya reservoir for intraventricular chemotherapy.
Two prospective studies on the survival of breast cancer patients with LMC compare systemic chemotherapy and radiation therapy with additional intra-CSF chemotherapy1213). Both studies report that intra-CSF chemotherapy does not prolong patient survival and significantly increases associated neurotoxicities. However, in both studies, systemic chemotherapy is not clearly defined, but described as 'appropriate chemotherapy'. Furthermore, ill-defined delayed neurotoxicity was unable to be differentiated from disease progression.
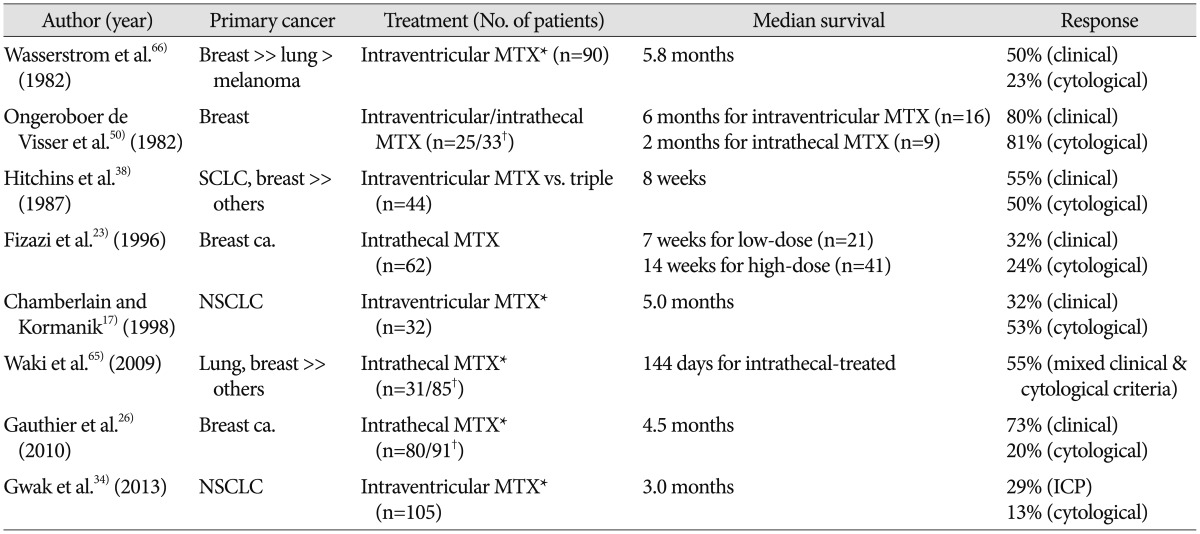
Clinical studies reporting results of intra-CSF chemotherapy
Although well-controlled, prospective or randomized study to evaluate the benefit of intra-CSF chemotherapy are lacking, intra-CSF can evidently prolong OS of patients with LMC, as compared to the untreated (Table 1)1723263438506566). However, such studies are limited by factors such as the small number of patients, heterogeneous primary cancer, different systemic cancer burdens, and various rounds of intra-CSF chemotherapy. Findings of previous studies show that 1) primary cancer of breast has a favorable prognosis as compared to lung cancer and/or melanoma, 2) more aggressive intra-CSF chemotherapy regimen/schedules show prolonged survival as a benefit of repeated treatment, and 3) increased intracranial pressure indicating a disrupted physiologic CSF flow is not only a bad prognostic factor but also a major obstacle to intra-CSF chemotherapy. Chamberlain and Kormanik17) report clinical results of 32 LMC patients from NSCLC after a relatively intense schedule of intraventricular chemotherapy, in which median survival is prolonged to 5 months. The 'intense schedule' includes the 'concentration×time' schedule administration of MTX (2 mg for 5 consecutive days every other week for 8 weeks), the second (cytosine arabinoside) and the third (Thiotepa) salvage intraventricular chemotherapy. In our study on the institutional data, median survival of 105 patients with LMC from NSCLC, who underwent a median 5 rounds of intraventricular chemotherapy via Ommaya reservoir, is 3.0 months34). Although the median OS is not impressive, we show the efficacy of intraventricular chemotherapy for patient survival using 'time-dependent covariate analysis' to eliminate the possibility of higher frequency chemotherapy given to patients who lived longer (the reverse-causation problem)34).
Due to the rarity of available drugs for intra-CSF chemotherapy, MTX in combination with or salvaged by cytosine arabinoside (Ara-C) with hydrocortisone or Thiotepa comprises most treatment regimens (Table 1). Although some patients with contraindications or resistance to MTX have some benefit from Ara-C or Thiotepa, it is still unclear whether MTX in combination with other drugs is superior to MTX monotherapy as the 1st line therapy3841). One randomized controlled study compares DepoCyt (sustained-release formulation of cytarabine; 50 mg every 2 weeks) to conventional intra-CSF MTX (10 mg twice a week for 4 weeks) in patients with LMC from solid tumors. Apparent prolonged OS in DepoCyt-treated patients (105 days vs. 78 days) has no statistical significance, but time-to-neurological progression is significantly delayed (58 days vs. 30 days)27).
REMAINED PROBLEMS IN THE INTRAVENTRICULAR CHEMOTHERAPY FOR LMC
Diagnosis and Treatment dk response measurements
LMC is defined as malignant cells in the CSF on cytology ex-amination. However, pathologic process usually occurs in the subpial CSF space, where cancer cells get lodged and cause neurological dysfunction and CSF flow obstruction. Hence, the low probability of floating cancer cells within a small amount of CSF results in 50-60% sensitivity of single CSF cytology despite overt LMC-related symptoms2866). Nevertheless, we obtain a sensitivity of 85-90% on repeated cytology examinations.
T1-weighted gadolinium enhancement MRI (Gd-MRI) of both brain and spine is the standard diagnostic procedure for patients with LMC to support the diagnosis and assess the extent of disease, including bulky disease293059). Although the 'evident enhancement of leptomeninges' on Gd-MRI reveal a sensitivity around 70% for diagnosis of LMC, the sensitivity may be as high as 90%. This is because it frequently contains 'suggestive findings' of enhancement of dura, ventricular ependyma with or without ventriculomegaly or nodular enhancement in subarachnoid space in patients with overt LMC-related symptoms2568). Combined with clinical features of LMC, Gd-MRI can support a diagnosis of LMC in patients with negative CSF cytology2556). Thus, in patients with known primary cancer who show suspected symptoms of LMC, Gd-MRI should be done before painful lumbar puncture, as it mimics leptomeningeal enhancement along with the infectious condition of CSF2947).
In context of the false negative CSF cytology for diagnosis, one-time negative conversion of CSF cytology after intra-CSF chemotherapy does not constitute a treatment response. Chamberlain and Kormanik17) propose complete response of CSF cytology as 'two consecutive negative results at least one week apart and sustained for at least one month' and partial response as 'from positive to suspicious' under the same conditions. However, these CSF responses are neither correlated with patients OS nor sustained for several months in patients with LMC from solid cancers, in contrast to prolonged CSF negative conversion in patients with leukemia at chemo-off period113456).
Rarity of drugs available for intra-CSF chemotherapy
While direct injection of drugs into CSF space bypasses the BBB, the risk of arachnoiditis requires available drugs to be water-soluble. Simultaneously, to avoid acute neurotoxicity from direct absorption into brain parenchyma, drugs should have appropriate chemical properties for intra-CSF use. Blaney et al.9) summarize characteristics of an ideal new agent for intrathecal administration as follows : 1) absence of neurotoxicity following systemic administration, 2) a mechanism of action that differs from agents currently available for intrathecal use or a novel mechanism of action, and 3) solubility in a vehicle that is suitable for intrathecal administration. Agents that meet the above conditions require intensive preclinical study including in vitro cytotoxicity, pharmacokinetics and chronic dosing study in the non-human primate before clinical trials.
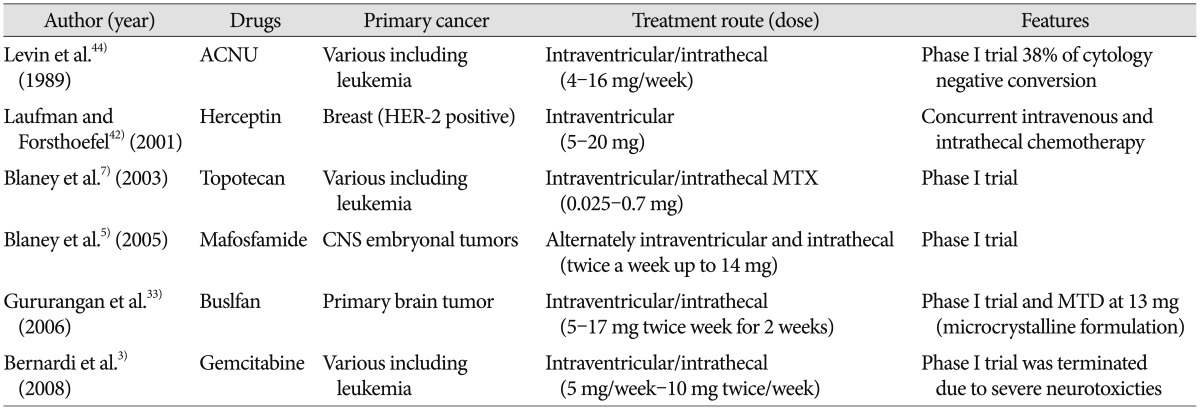
RECENTLY INTRODUCED CYTOTOXIC DRUGS FOR INTRA-CSF CHEMOTHERAPY
List and clinical results are summarized in Table 2.
Topotecan
Topotecan, a topoisomerase I inhibitor shows a wide-spectrum of anti-tumor activity. While it has a relatively high CSF penetration rate (30%), systemic or central nervous system (CNS) toxicity is rarely observed. These properties suggest the intrathecal use of topotecan, and non-human primate pharmacokinetic study show a 450-fold higher CSF concentration after an intraventricular dose of 0.1 mg than systemic administration6). Subsequently, phase I trial was performed in patients with LMC from various cancers including leukemia, breast cancer, lung cancer and gliomas7). At a maximal tolerable dose (MTD) of 0.4 mg, lumbar CSF concentration at 2 hours is 1 uM at an average 15% of ventricular concentration. Among the 23 patients ob-served, grade 3 transient arachnoiditis occurred in 3 patients and 1 patients showed grade 3 ataxia, which did not completely recover. All 3 leukemia patients and 3 of the 13 glioma patients showed CSF cytology responses but following phase II study is not yet performed.
Mafosfamide
Mafosfamide is a preactivated formulation of cylophsophamide, which shows wide spectrum anti-tumor activity but typically needs hepatic enzyme activation to become cytotoxic. As cyclophosphamide is effective for CNS embryonal tumors, which have a predilection for LMC, clinical trials are performed on young children with these tumors to prevent LMC and to delay or possibly avoid whole neuraxis radiation. Initial phase I study failed to achieve cytotoxic CSF concentration (>10 uM) due to dose-limiting toxicity (DLT) of headache and/or irritability and rapid clearance at 5 mg of mafosfamide4). However, in the following phase I study, patients could tolerate 14 mg of mafosfamide with premedication of steroid and morphine and had effective mafosfamide CSF concentration5). The recently published result of 'systemic and intrathecal mafosfamide followed by conformal radiation for infants with intracranial CNS tumor : a pediatric brain tumor consortium study (PBTC-001)' suggest that the incopration of intrathecal mafosfamide to systemic chemotherapy is feasible8).
Gemcitabine
Gemcitabine, a deoxy-citidine analog anti-metabolite, shows anti-tumor activity against various solid tumors. As gemcitabine is water-soluble but barely penetrates blood-CSF barrier after intravenous administration, it is considered as an excellent candidate for intrathecal chemotherapy. Non-human primate study of intraventricular gemcitabine administration is promising as it reveals negligible plasma gemcitabine concentration with effective CSF concentration based on pharmacokinetics22). On 5 mg per week for 4 weeks schedule, there is no discernible neurotoxicity except transient CSF pleocytosis. Thus, a phase 1 clinical trial has been launched with a basal dose of 5 mg per week (1/10th of the non-human primate dose equivalent based on the different CSF volume)3). However, DLT of 2 severe neurotoxicities (transverse myelitis and somnolence) occurred at the 10th and 7th administration of intrathecal gemcitabine without objective response other than stable disease. Phase I trial is prematurely discontinued due to different cytidine deaminase (converting gemcitabine to its inactive form) levels between non-human primates and human, lack of chronic dosing study, and prior treatment of intrathecal chemotherapy and radiation in patients show DLTs.
Busulfan
Non water-solubility of busulfan precludes its intrathecal administration while it shows activity against cyclophosphamide resistant neoplasms. Microcrystalline formulation (Starject bu-sulfan®, SuperGen Inc., San Ramon, CA, USA) solves the solubility problem, and successful intrathecal Starject busulfan in a nude rat model has prompted phase I clinical trial in children with primary brain tumors (PBTC-004)33). Effective CSF con-centration of 50-150 ug/mL is achieved with transient grade 3 toxicities of vomiting, headache and arachnoiditis on a 5-17 mg twice weekly for 2 weeks schedule; 13 mg of busulfan is recom-mended for future phase II study.
ACNU (3-[(4-amino-2-methyl-5-pyrimidinyl)methyl]-1-(2-chloroethyl)-1-nitrosourea hydrochloride)
Levin et al.43) tested chloroethy nitrosoureas, which have ad-vantage of non-cell cycle specific agents, in a beagle model. Among the nitrosureas, water-soluble ACNU is best tolerated, and based on the observed clearance rate, the phase I baseline dose of 8 mg/week every other week is suggested44). Accumulated dose of up to 104 mg (8 mg per week×13 times) leads to no bone marrow suppression in patients. Neurotoxicities of headache, nausea, vomiting, and radiculopathy are all transient.
MONOCLONAL ANTIBODIES AND TARGET INHIBITORS FOR INTRA-CSF CHEMOTHERAPY
Monoclonal antibodies
As monoclonal antibodies do not cross the BBB due to molecular weight, successful intrathecal Rituximab treatment in lymphoma and leukemia has prompted the introduction of monoclonal antibodies to intra-CSF chemotherapy. Among these, Hereptin (transtuzumab) is the most widely used monoclonal antibody targeting LMC from HER-2 positive breast cancer. Despite the absence of systematic phase I trial, single dose is escalated up to 150 mg but the interval is variable according to case reports39). A pooled analysis of intrathecal Herceptin reveals 2/3rd CSF response, median OS of 13.5 months and median PFS of 7.5 moths69). Other monoclonal antibodies, combined with immunotoxin or radio-isotope to increase cancer cell specificity or lethal effect are tried in animal models but not in human yet.
Receptor tyrosine kinase inhibitors
Recent studies report that patients with LMC from NSCLC, who receive intrathecal or intraventricular chemotherapy with concurrent RTKi, have prolonged survival compared to patients with intra-CSF chemotherapy alone345167). RTKi's partially cross the BBB and oral dose regimen of erotinib and gefitinib achieve effective CSF concentration in this low bound-protein compartment204046). Frequent clinical response in patients with parenchymal brain metastasis and/or LMC from NSCLC after RTKi, is an impetus to evaluate its efficacy in further clinical trials according to EGFR mutation.
VENTRICULO-LUMBAR PERFUSION TO OVERCOME CSF FLOW DISTURBANCE
CSF flow obstruction, found in >50% LMC patients, is a long standing major obstacle to intraventricular chemotherapy as it hinders effective distribution of injected drugs16). Most studies measuring ICP in LMC patients agree that increased ICP is one of the poor prognostic factors for patient survival183234). Compartment model of CSF flow predicts that simple diffusion cannot achieve even distribution of injected drugs in case of disturbed CSF flow, as the diffusion distance between the ventricle and lumbar subarachnoid space is too long to be reached without physiologic CSF flow10). As a consequence, increased gradient and transit time of injected drugs in the lateral ventricle facilitate penetration into brain parenchyma and causes encephalopathy3132). Siegal et al.56) report that the incidence of delayed leucoencephalopathy in LMC patients treated with intraventricular chemotherapy significantly correlates with increased ICP.
Perfusion of chemotherapeutic drug from one lateral ventricle to another or lumbar space was tried by Rubin et al.52) for the purpose of treating glioma or meningeal leukemia while reducing systemic absorption. Later, Nakagawa et al.49) attempt "ventriculolumbar perfusion" (VLP) chemotherapy to increase drug delivery to the lumbar subarchnoid space. MTX is injected into the ventricle as a bolus while artificial CSF is perfused from the ventricle to lumbar drainage for 3 days on VLP in LMC patients from solid cancers (Fig. 1). While 3 out of 6 bed-ridden patients unexpectedly achieved ambulation after VLP, all 13 patients transiently suffered from severe nausea, vomiting, headache, fever, and confusion. Nakagawa et al.49) propose further investigation to establish appropriate drug doses and perfusate volume, while they stop VLP due to the unacceptable toxicities as com-pared to standard intrathecal chemotherapy. A phase I study of VLP by Gwak et al.36) suggests both perfusion rate and daily MTX dose as variables for MTD. They introduce a continuous infusion of MTX and artificial CSF mixture to human clinical trial for the first time with proven effective CSF concentration at a lower dose of MTX than bolus injection in the non-human primate model1). Perfusion rate of 20 mL/h and daily MTX dose of 24 mg is well-tolerated in patients. The surprising control rate of increased ICP (75%) has prompted phase II trial of VLP. Subsequent phase II trial shows significantly high control rate of increased ICP (71% in 45 patients, median time-to ICP control of 104 days) and prolonged OS of 6.0 moths with 19% of improved ambulatory function including 4 bed ridden patients who became ambulatory. The study shows that the OS of NSCLC patients with LMC is double that of conventional NSCLC patients with LMC (3.0 months vs. 6.0 months, p<0.001). VLP thus shows following advantages 1) VLP can be applied to patients with increased ICP, for whom conventional intra-CSF therapy cannot be applied or is ineffective, 2) both symptom improvement rate and OS is significantly improved in these patients who have bad prognostic clinical factors. Further investigation to reduce the constitutive side effects of VLP (nausea, vomiting and confusion) by reducing perfusion rate is on-going.
FUTURE DIRECTIONS INCLUDING BIOLOGICAL/PHARMACODYNAMIC MARKERS
As CSF cytology shows frequent false negative results, investigators have sought more predictive diagnostic values for CSF profiles such as elevated protein levels, low glucose, and increased lactate dehydrogenase/β-glucosidase/β-2 microglobulin etc. or a combination of these values37636465). However, they are consistent with, but not diagnostic of LMC, and investigators are un-able to provide cut-off values of the diagnostic variables agreeable to clinicians. Tumor specific antigens such as CA 19-9, Cyfra 21-1 or CEA have higher sensitivity and specificity than CSF cytology or other markers265364). But, they do not appear in all patients that have these primary cancers. Recent efforts to find a small amount of onco-protein, onco-DNA or onco-microRNA in CSF utilizing advances in molecular biological techniques show promising results2455860), but the pilot studies need to be validated in a large number of patients including a control group.
We also need a pharmacodynamic marker for intra-CSF chemotherapy to monitor the treatment response and to set a therapeutic end point. However, current CSF cytology examination is neither valid for complete/partial remission nor appropriate for quantitative measurement of cancer cell burden. Quantitative measurement of cancer metabolites or exosomes is on-going, but a correlation with clinical status is not yet proven4562). Subpial deposit of cancer cells is more commonly found than free floating cells in the CSF flow, hence simple measurement of CSF values does not fully represent the cancer cell burden of LMC. Thus, elaborate analyses of these variables should combine clinical information such as the post-treatment time of CSF sample and the patient's clinical status.
CONCLUSION
Prognosis of patients with LMC from solid tumors is still dismal without a cure despite intra-CSF chemotherapy. However, major problems of intra-CSF chemotherapy can be solved by developing more available drugs to overcome drug-resistance and advancement of drug delivering technique such as VLP. Elaborate search for biomarker/pharmacodynamic marker combined with clinical findings would greatly facilitate the introduction of new drugs and technologies to clinical trials for LMC.