Comparison of Morphological Characteristics of the Subaxial Cervical Spine between Athetoid Cerebral Palsy and Normal Control
Article information
Abstract
Objective
To compare the morphometry of subaxial cervical spine between cerebral palsy (CP) and normal control.
Methods
We retrospectively analyzed 72 patients with CP, as well as 72 patients from normal population. The two groups were matched for age, sex, and body mass index. Pedicle, lateral mass (LM), and vertebral foramen were evaluated using computed tomography (CT) imaging. Pedicle diameter, LM height, thickness, width and vertebral foramen asymmetry (VFA) were measured and compared between the two groups. Cervical dynamic motion, disc and facet joint degeneration were investigated. Additionally, we compared the morphology of LM between convex side and concave side with cervical scoliotic CP patients.
Results
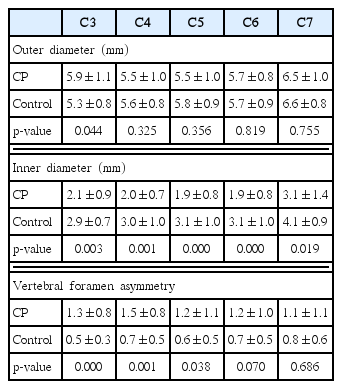
LM height was smaller in CP group. LM thickness and width were larger in CP group at mid-cervical level. In 40 CP patients with cervical scoliosis, there were no height and width differences between convex and concave side. Pedicle outer diameter was not statistically different between two groups. Pedicle inner diameter was significantly smaller in CP group. Pedicle sclerosis was more frequent in CP patients. VFA was larger in CP group at C3, C4, and C5. Disc/facet degeneration grade was higher in the CP group. Cervical motion of CP group was smaller than those of the control group.
Conclusion
LM morphology of CP patients was different from normal population. Sclerotic pedicles and vertebral foramen asymmetry were more commonly identified in CP patients. CP patients were more likely to demonstrate progressive disc/facet degeneration. This data may provide useful information on cervical posterior instrumentation in CP patients.
INTRODUCTION
Athetoid cerebral palsy (CP) is a static encephalopathy caused by neonatal hypoxia occurring during the perinatal or postnatal phases of development. Early onset of extensive spondylosis of the cervical spine, deformity and instability due to sustained abnormal muscular tonicity, or excessive movement of the neck are found in patients with athetoid type of cerebral palsy2,6,10). And many of them progressively more disabled and surgical treatment is usually required.
Several surgical procedures have been described; in the earlier era of the operation for cervical spondylotic myelopathy associated with cerebral palsy, decompressive laminectomy was frequently performed, but it caused spinal instability and consequent recurrence of symptoms2,12). For these reasons, cervical instrumentation and fusion are essential.
Clinically, there are many characteristic features of patients with athetoid cerebral palsy compared to normal population including dystonic athetoid neck movements2,4,6). Morphological characteristics of cervical spine in CP patients are different from those of normal patients. As a result, a better understanding of the morphological characteristics of the cervical spine in patients with CP would be important to surgeons performing safer and more accurate instrumentation. The aim of this study was to compare the morphometric subaxial cervical spine between patients with athetoid cerebral palsy and normal population.
MATERIALS AND METHODS
After Institutional Review Board approval, we retrospectively reviewed radiologic study of 72 patients with CP, as well as 72 normal controls without cerebral palsy. The two groups underwent multiplanar computed tomography (CT) and an X-ray of the cervical vertebrae from 2006 to 2014. We compared the morphological characteristics of subaxial cervical spine between two groups.CP group included 32 males and 40 females. Their mean age was 42.6 years (range, 22–74 years) at the time of cervical radiological evaluation. Mean body mass index (BMI) was 21.6 (range, 17.8–24.2). Among them, 21 patients had received instrumentation and fusion surgery for cervical compressive myelopathy due to subaxial lesion. For these patients, we reviewed the preoperative radiologic study. The control group included 32 males and 40 females who checked CT scan due to the mild trauma without any history of cervical spine disease. Each patient in the control group was matched to the age and BMI of a CP patient. Mean age in the control group was 44.2 years (range, 24–76 years) and mean BMI was 21.5 (range, 17.5–23.8).
Both groups underwent standardized axial bone-window CT scanning and a plain X-ray of cervical spine. All CT scans were performed on a Siemens 64-slice CT scanner with 3-mm axial image thickness (Siemens Medical Solutions, Erlangen, Germany). Sagittal and coronal reconstructions were obtained using 1.25-mm thickness slices. CT films were scanned at a resolution of 512×512 pixels, a field of view of 180 mm, and CT interactive software was used to edit the images. Linear and angular measurements were made using m-view 5.4 software (Marosis Technologies Inc., Seoul, Korea).
Lateral mass
We performed a morphometric analysis of the lateral masses from C3–C7 by taking measurements of anterior height (LMAH), posterior height (LMPH), thickness (LMT), width (LMW) on a true axial, and sagittal CT slice that passed by the center of the lateral mass. LMAH was the distance between the two adjacent joints on the anterior aspect of the lateral mass and LMPH was the distance between the two adjacent joints on the posterior aspect of the lateral mass. LMT was the distance between the dorsal and ventral cortices of the center of the lateral mass and LMW had the largest width of lateral mass on axial CT image (Fig. 1). We compared the morphology of subaxial lateral masses (LMAH, LMPH, LMT, and LMW) between convex side lateral mass and concave side lateral mass with cervical scoliotic CP patients. In 30 patients, cervical coronal scoliosis was confirmed. Cervical coronal scoliosis was defined as coronal Cobb’s angle greater than 10° on an anterior-posterior plain cervical X-ray.
A schematic diagram of the lateral mass, pedicle and vertebral foramen asymmetry parameters measured on computed tomography scans. LMAH : lateral mass anterior height, LMT : lateral mass thickness, LMPH : lateral mass posterior height, a : distance from the midline to right vertebral foramen, b : distance from the midline to left vertebral foramen, POD : pedicle outer diameter, LMW : lateral mass width, PID : pedicle inner diameter.
Pedicle and transverse foramen
On the surfaces that passed the axes of bilateral pedicles, the pedicle outer diameter (POD), and inner diameter (PID) of both pedicles in C3 to C7 were measured. POD was outer cortical diameter and PID was inner cancellous diameter (Fig. 1). Vertebral foramen asymmetry (VFA) was evaluated in C3 to C6 by measuring the difference between the left and right distance from the midline (Fig. 1). C7 was excluded because of absence or hypoplasia of vertebral foramen.
Degeneration of disc and facet joint
Degeneration of cervical discs from C3 to C7 was graded on lateral cervical radiographs. The grading of cervical disc degeneration was based on the grading system previously described in Hilibrand et al.7) The degree of degeneration was graded into three categories : grade I, normal; grade II, narrowing of disc space and no posterior osteophytes; and grade III, less than 50% of normal disc space height and posterior osteophytes are present. The degree of cervical facet degeneration was bilaterally determined on CT from C3 to C7. The grading of cervical facet degeneration was based on the grading system previously described in Park et al.19). The degree of degeneration was graded into four categories : grade I, normal; grade II, degenerative changes including joint space narrowing, cyst formation, small osteophytes without joint hypertrophy seen on axial or sagittal images; grade III, joint hypertrophy secondary to large osteophytes without fusion on axial or coronal images; and grade IV, bony fusion of the joint seen on sagittal images.
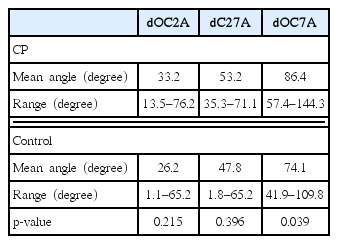
Cervical spine motion
We reviewed dynamic lateral plain X-rays for the comparison of cervical dynamic motion range between the two groups by measuring occipital–C2 angle (O–C2A), C2–C7 angle (C2–7A), and occipital–C7 angle (O–C7A). The O–C2A indicates the angle between McGregor’s line and the inferior vertebral endplate line of C220). The C2–C7A indicates the angle between the inferior endplates of the C2 and C7 vertebral bodies. The O–C7A indicates the angle between McGregor’s line and the inferior vertebral endplate line of C7. The differences in the O–C2A (dOC2A), C2–C7A (dC27A), O–C7A (dOC7A), i.e., the differences between the values in the flexion and the value in the extension position, were calculated for both groups (Fig. 2).
Dynamic lateral plain X-rays for cervical dynamic motion range. The O–C2A represents the angle between McGregor’s line and the inferior endplate of C2. The C2–7A represents the angle between the inferior endplates of C2 and C7. The O–C7A represents the angle between McGregor’s line and the inferior endplate of C7.
Statistical analysis
All analyses performed with the IBM SPSS Statistics software program version 18 (SPSS Inc., Somers, NY, USA). For the comparisons of the parameters between the groups, paired t-test for normally distributed continuous variables and Wilcoxon signed-rank test for non-normally distributed continuous variables was used and Fisher exact were used for categorical data. For all statistical tests, p<0.05 was considered to be significant.
RESULTS
A total of 144 lateral masses were compared between CP group and the control group. LMAH in CP group was ranged from 7.8 to 15.8 mm and it was found to be smaller than that in the control group on all cervical levels (p<0.01, Fig. 3). LMPH in CP group ranged from 7.1 to 15.7 mm and was found to be smaller than that of the control group at C3, C4, and C5 (p<0.01). LMT in CP group was ranged from 5.2 to 18.5 mm and was found to be larger than that of the control group at C3 and C4 (p<0.01 and p=0.02, respectively). At C5, C6, and C7, there was no difference between two groups in terms of LMT. Also, LMW in CP group was ranged from 9.0 to 18.5 mm and was found to be larger than that of the control group on all levels (p<0.05) except for C7 (Table 1). For 40 patients in CP group with cervical scoliosis, there were no significant differences of LMAH, LMPH, LMT, LMW between convex side lateral mass and concave side lateral mass (p>0.05).
Parasagittal computed tomography reconstruction images show lateral mass height of cerebral palsy group (A) is smaller than that in the control group (B) on all cervical levels.
POD in CP group ranged from 2.7 to 8.5 mm and no significant differences were observed with POS of the control group on all cervical levels. PID in CP group ranged from 0.3 to 6.3 mm and was found to be smaller than that of the control group on all cervical levels (p<0.05, Table 2). Pedicle sclerosis is identified in the 12 patients of the CP group. However there was only one pedicle sclerosis in normal control group (16.7% vs. 1.4%, p<0.01, Fig. 4). VFA in CP group ranged from 0 (symmetric vertebral foramen from midline) to 4.4 mm and was found to be larger than that of the control group at C3, C4, and C5 (p<0.05). At C6, VFA had a tendency for increase compared to the control group (p=0.07), but this difference was not statistically significant (Table 2).
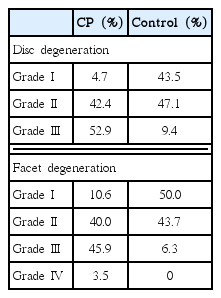
When comparing cervical disc degeneration grade and facet degeneration grade, the patients in CP group were statistically more likely to demonstrate progressive disc degeneration than the patients in the control group (p<0.01). Disc degeneration above grade II accounted for 95.3%. Facet degeneration in CP group was statistically more progressed than in the control group (p<0.01). Facet degeneration above grade II accounted for 89.4% (Table 3).
The mean value of dOC2A in CP group was 26.2° in the range from 1.1° to 65.2°; the mean value of dC27A in CP group was 47.8° in the range from 1.8° to 65.2°; both values were smaller than the corresponding values in the control group, although the differences did not reach statistical significance. The mean value of dOC7A in CP group was 74.1° in the range from 41.9° to 109.8° and was found to be significantly smaller than that of the control group (p=0.039, Table 4).
DISCUSSION
Early onset of cervical degeneration due to sustained abnormal tonicity or movement of the neck was found in the patients with cerebral palsy. In surgery, several studies reported that decompression without fusion or laminoplasty is not recommended because of repetitive cervical abnormal movement, adjacent segment instability, and progression of spondylosis13,17,18,22). Therefore, rigid instrumented fixation is required to obtain satisfactory outcome.
Since the advent of cervical lateral mass screw fixation by Roy-Camille et al.21) in 1972, several techniques for lateral screw placement are available, including Roy-Camille, Louis, Magerl, Anderson techniques1,8,16). The anatomic structures at risk during lateral mass screwing of the cervical spine are the nerve roots, the vertebral arteries, and the adjacent lateral masses3). The lateral mass screw fixation is safer than the cervical pedicle screw fixation; however, if the lateral mass is small or if the lateral mass or facet joint has been fractured, the lateral mass screw fixation may entail the problem of screw loosening or avulsion9,14,16). Furuya et al.4) reported that subaxial pedicle instrumentation contribute to the achievement of relatively good surgical outcomes for CP patients. Several studies reported that abnormal neck motion of CP patients accelerates degenerative change of cervical spine9,22). Harada et al.5) reported that the cervical spine in patients with CP is characterized by vertebral body flattening and a narrow sagittal spinal canal diameter. Kato et al.9) reported that pedicle sclerosis, a wide transverse angle, and a lateral mass deformity were frequently observed in patients with CP. Our study described the morphological characteristics of subaxial cervical spine in patients with athetoid CP compared with age-, BMI-matched normal population for safe cervical instrumentation.
This study first described the morphological characteristics of lateral mass in patients with CP. Superior-inferior mean diameter (LMAH and LMPH) of CP group ranged from 10.8 to 12.6 and was smaller than that of the control group. These findings mean that lateral mass of CP patients is superior-inferiorly smaller and anterior-posteriorly, mediolaterally larger than that of normal population especially in the mid-cervical spine. So, selection of the entry point and sagittal angulation may be important to avoid facet joint violation during the lateral mass screw placement in the CP patient. Also, these data indicate that the greater stress is generated at the mid-cervical spine than the lower cervical spine in the CP patient. The sudden increase in size at C6 and C7 of the vertebral bodies and spinous processes in the human cervical spine may explain this finding because the shearing stress per area unit becomes bigger as the vertebra decreases in size. Furthermore, there was no directional difference of lateral mass degeneration for CP patients of cervical scoliosis. This means, for CP patients, abnormal neck motion worsens cervical degeneration on both concave and convex sides. In this study, we found that the mean pedicle outer diameter in CP group was 5.5 to 6.6 mm and the outer diameter was not different from that of the control group except for C3. The mean outer diameter in the control group was 5.3 to 6.6 mm and it was similar to the outer diameter measured by CT in Kato et al.9). The mean inner diameter in the control group was 1.9 to 3.1 mm and the inner diameter was smaller than that of the control group on all subaxial cervical levels. Pedicle sclerosis was frequently observed in patients with CP as well. This finding suggests that the safety margin for pedicle screw fixation could be narrower in the CP group compared with the normal population. Two studies reported that the breach rate was higher in patients with CP because of loss of anatomical landmarks in a vertebra and the osteosclerotic changes of the pedicle14,15). Therefore, cervical pedicle screw instrumentation could be dangerous especially for CP patients with massive spondylosis.
Regard to the vertebral foramen asymmetry of CP patients, in CP group, the mean difference value between the left and right distance from the midline was larger than 1mm, whereas it was smaller than 1mm for the control group. Our results indicate that vertebral foramen of subaxial cervical spine of CP patients is more asymmetric than that of normal population. We suppose that vertebral foramen asymmetry is associated with massive degeneration of cervical spine of CP patients.
In this study, patients in CP group were more likely to demonstrate progressive disc, facet degeneration than patients in the control group. Harada et al.5) reported that disc degeneration occurred earlier and progressed more rapidly in the patients with advanced disc degeneration in 51%, i.e., eight times the frequency in normal subjects. In our study, severe disc degeneration above grade III was observed in 52.9% of cases in CP group, similarly to previous reports. We graded the degree of facet degeneration into four categories. Park et al.19) reported that greater than grade III facet joint arthrosis was common in patients older than 60 years old and at C2–C3, C3–C4, and C4–C5. In our study, facet degeneration above grade III was observed in 49.4% of CP group. Facet degeneration occurred earlier and progressed more rapidly in the patients of CP. We suppose that disc and facet degeneration were aggravated by sustained muscular tonicity and excessive movement of the neck in CP patients.
CP patients show various involuntary movements of the neck, face, arms, and upper body. Previously, it was erroneously assumed that cervical motion range of CP patients was larger than normal population. By contrast, the results of the present study show that cervical neck motion range of CP group was smaller than that of the control group. Although not statistically significant, dOC2A and dC27A of CP group were smaller than those of the control group. However, dOC7A was significantly smaller than that of the control group. Phillips et al.20) reported that, in the measurement of C0–C2 angle differences between flexion and extension X-ray, the mean value of C0–2 angle differences in healthy patients was about 33° and larger than that of CP group. Kim et al.11) reported the measurement of C2–C7 angle differences between flexion and extension X-ray for 105 patients with symptomatic single or two-level cervical disc disease. The mean value of C2–7 angle differences in cervical disc patients was about 50° and larger than that of CP group. We suppose that the decrease of cervical dynamic motion is associated with disc, facet joint degeneration of cervical spine of CP patients. Further research is required for cervical dynamic motion changes in CP patients.
This study has several limitations. First, the number of patients included in this study was limited because of the small number of CP cases. Second, although the two groups were matched for age and BMI, the height and weight of CP group was not exactly matched to those of control group. Third, we could not explain the mechanism between cervical morphological changes and involuntary movement in CP patients. Further research, including a closer inspection of the reasons underlying this mechanism, is necessary.
CONCLUSION
CP patients were more likely to demonstrate progressive morphological degeneration than normal population. Lateral mass morphology in patients with CP was different from that in normal population. Although longer lateral mass screw could be acceptable in CP patients compared to the normal control, however the selection of the accurate entry point and sagittal angulation is important to avoid facet joint violation during the lateral mass screw placement in the CP patient. Sclerotic pedicles and vertebral foramen asymmetry were more frequently identified in CP patients. Pedicle screw placement in a sclerotic pedicle and narrow pedicle could be associated with a higher risk of misplacement. So, preoperative imaging study is critically important to decide the method of posterior instrumentation for the patients with CP.
Notes
CONFLICTS OF INTEREST
The authors have no financial conflicts of interest.
INFORMED CONSENT
Informed consent was obtained from all individual participants included in this study.