Acute Contralateral Radiculopathy after Unilateral Transforaminal Lumbar Interbody Fusion
Article information
Abstract
Objective
Cases of contralateral radiculopathy after a transforaminal lumbar interbody fusion with a single cage (unilateral TLIF) had been reported, but the phenomenon has not been explained satisfactorily. The purpose of this study was to determine its incidence, causes, and risk factors.
Methods
We did retrospective study with 546 patients who underwent a unilateral TLIF, and used CT and MRI to study the causes of contralateral radicular symptoms that appeared within a week postoperatively. Clinical and radiological results were compared by dividing the patients into the symptomatic group and asymptomatic group.
Results
Contralateral symptoms occurred in 32 (5.9%) of the patients underwent unilateral TLIF. The most common cause of contralateral symptoms was a contralateral foraminal stenosis in 22 (68.8%), screw malposition in 4 (12.5%), newly developed herniated nucleus pulposus in 3 (9.3%), hematoma in 1 (3.1%), and unknown origin in 2 patients (6.3%). 16 (50.0%) of the 32 patients received revision surgery. There was no difference in visual analogue scale and Oswestry disability index between the two groups at discharge. Both preoperative and postoperative contralateral foraminal areas were significantly smaller, and postoperative segmental angle was significantly greater in the symptomatic group comparing to those of the asymptomatic group (p<0.05).
Conclusion
The incidence rate is not likely to be small (5.9%). If unilateral TLIF is performed for cases when preoperative contralateral foraminal stenosis already exists or when a large restoration of segmental lordosis is required, the probability of developing contralateral radiculopathy is increased and caution from the surgeon is needed.
INTRODUCTION
Blume and Rojas2) first published in the 1980s a modified unilateral approach of posterior lumbar interbody fusion (PLIF), named transforaminal lumbar interbody fusion (TLIF). Harms and Jeszensky12) confirmed its treatment outcome and contributed to the popularization of TLIF during the 1990s. Humphreys et al.18) and Hankenberg et al.11) reported that TLIF led to minimal loss of normal structure compared with PLIF, and that it showed no differences in blood loss, operation time, and hospital day. Recently, TLIF has shown a high success rate and a low complication rate, and it has been widely used as an effective treatment for various degenerative lumbar spinal disorders1114202526).
When initially performing TLIF, two cages were usually inserted through bilateral approaches212). As there have been several reports that unilateral cage showed no significant difference in treatment outcome and complications compared with bilateral cage and that it is biomechanically stable, TLIF with a single cage (unilateral TLIF) has been performed widely in recent years38). In the unilateral TLIF, the approach side is decided according to the side of the patient's symptom. On the other hand, contralateral foramen can be indirectly decompressed by increased disc height with a single cage inserted in the ipsilateral side1720). However, Hunt et al.19) recently reported a case showing postoperative contralateral side leg pain as a complication of a unilateral TLIF. Although the authors did not present precise data, they hypothesized that an increase of lordosis during surgery might have effect on contralateral foraminal stenosis and contralateral leg symptoms.
Despite the possibility of developing contralateral radicular symptom after a unilateral TLIF, there have been no studies analyzing causes of this phenomenon. We tried to investigate risk factors to find out causes of contralateral radiculopathy after a unilateral TLIF in this study.
MATERIALS AND METHODS
Patient populations
We did a retrospective study with patients who received TLIF in the L1-S1 area between January 2005 and December 2013. We performed unilateral TLIF for a total of 592 patients, complaining low back pain and unilateral radicular symptoms, under diagnosis of degenerative stenosis with ipsilateral foraminal stenosis, spondylolisthesis, and repeated postoperative herniated nucleus pulposus (HNP). Patients with congenital or degenerative spinal deformities were not included in the study group. We performed bilateral TLIF and decompression for the patients with bilateral radicular symptoms, who were not included in this study either. A total of 546 patients were enrolled in this study excluding 46 patients who received the operation upon a diagnosis of infectious spondylitis, spine tumor, or fracture at the index level.
MRI was performed for all patients who had radicular symptoms which did not solved with medication and nerve blocks for more than 1 month. CT was prescribed for the patients who were indicated for surgery according to the MRI findings. Foraminal stenosis was diagnosed as root compression and loss of perineural fat layer at the neural foramen on MRI. There was no foraminal stenosis on the contralateral side even though some patients had smaller contralateral foraminal area comparing to those of other asymptomatic levels.
The patients were divided into two groups : one group comprised those who presented with new leg symptoms including pain, hypoesthesia, paresthesia, and motor weakness, in the side contralateral to the original symptom side within 1 week after surgery (symptomatic group), and the other group comprised those without contralateral symptom after surgery (asymptomatic group).
Surgical techniques and postoperative management
Unilateral TLIF was performed by two different neurosurgeons. Their TLIF procedures are almost same. The patient was positioned with lumbar extension by placing pillows at the chest and pelvis. After midline vertical skin incision, unilateral partial laminectomy and facetectomy were done. Contralateral side decompression was not performed and the contralateral ligamentum flavum was saved in unilateral TLIF. After a meticulous endplate preparation for upper and lower endplates, disc space was filled with autologous bone chips from lamina and facet, and the CAPSTONER® PEEK cage (Medtronic Sofamor Danek Inc., Memphis, TN, USA) filled with the autologous bone chips was inserted obliquely. The cage was located in the center and crossed midline of the disc space. Pedicle screw fixation was done after the cage insertion. Rod compression was not performed routinely due to prevent contralateral foraminal stenosis where the decompression was not performed. The wound was closed after bilateral pedicle screw fixation.
Simple radiograph and CT were taken for all the patients with postoperative contralateral radicular symptoms. MRI was taken if further evaluation was needed additional to the CT study. Nerve blocks for medial branch and root were performed for initial pain control. Revision surgery was indicated in cases the nerve blocks were not effective. However, revision surgery was immediately performed when root compression was definitive on image studies or motor weakness was accompanied. Revision surgeries, such as facetectomy, discectomy, screw reposition, and hematoma removal, were done for the contralateral pathologies.
Causes of contralateral symptoms
The causes of contralateral symptoms in the symptomatic group were categorized into five, contralateral foraminal stenosis, newly developed HNP, screw malposition, hematoma, and unknown origin. Contralateral foraminal stenosis was defined as a decreased postoperative foraminal area (FA) compared with the preoperative value; HNP as a newly developed HNP on the side contralateral to the TLIF side; and screw malposition as invasion of contralateral pedicle screw into central canal or neural foramen. Hematoma meant epidural hematoma formed in the surgical wound compressing dural sac.
Clinical outcome
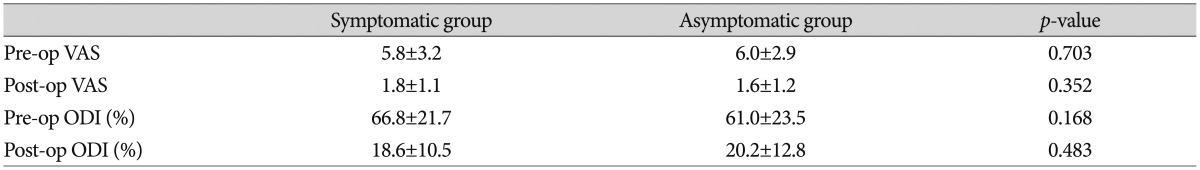
To assess the difference in clinical outcomes between the symptomatic and asymptomatic groups, visual analogue scale (VAS) scores and Oswestry disability index (ODI) were measured immediately before surgery and at 3 months after surgery.
Radiographic measurement
Disc height (DH), lumbar lordosis (LL), and segmental angle (SA) were measured with plain radiographs before and after the surgery. DH was defined as the distance between the upper and lower endplates at the center of the disc space at the index level. LL was measured as the angle between the two upper endplates of L1 and S1. SA was measured as the angle between the upper and lower endplates at the disc level where surgery was performed (Fig. 1)24). Postoperative changes of LL and SA were calculated by subtracting the preoperative angle from the postoperative angle in each group. Preoperative and postoperative DH, LL, and SA values were compared in each group, and postoperative changes of LL and SA were also compared. Contralateral foraminal areas (FA) were checked from preoperative and postoperative CT. FA (mm2) was defined as the area of bony neural foramen at the center of pedicle from the sagittal view of CT. Postoperative change of FA was measured as the difference between preoperative and postoperative FA's.
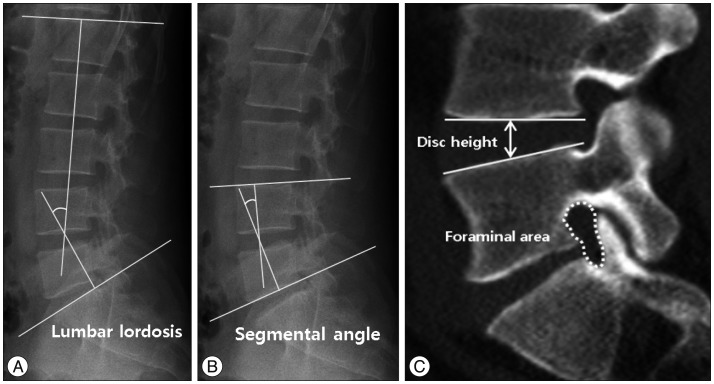
Measurement of lumbar lordosis, segmental angle, disc height and contralateral foraminal area. A : Lumbar lordosis : the angle between L1 and S1 upper endplates. B : Segmental angle : the angle between the upper and lower endplates at the disc space where surgery was done. C : Disc height: the distance between the upper and lower endplates at the center of the disc space at the surgical site from the sagittal view in the plain radiograph. Foraminal area : the area of bony neural foramen.
All the factors were measured 3 times blindly for patient information, and the mean values were used for this study.
Statistical analysis
Data obtained through the measured VAS and ODI scores and radiological analysis of LL, SA, and FA were analyzed for statistical significance by using Student's t-test, and a p-value of <0.05 was considered to be statistically significant.
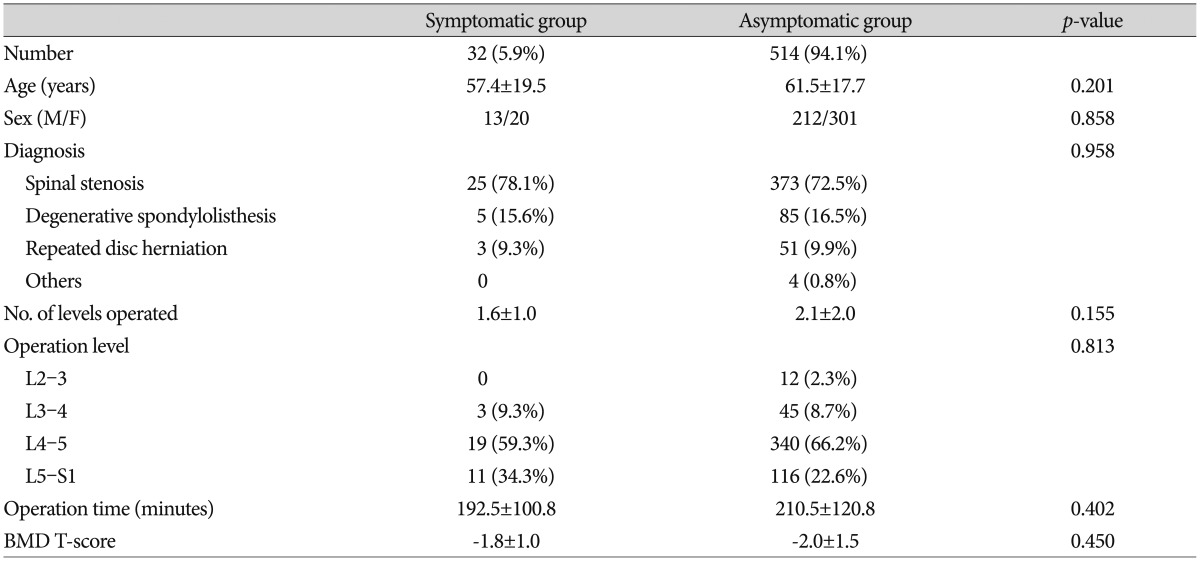
RESULTS
The incidence of contralateral radiculopathy after a unilateral TLIF surgery was 5.9% (32/546). There was no statistically significant difference in mean age, sex ratio, bone mineral density T-score, and the number of operated levels between symptomatic and asymptomatic groups (Table 1).
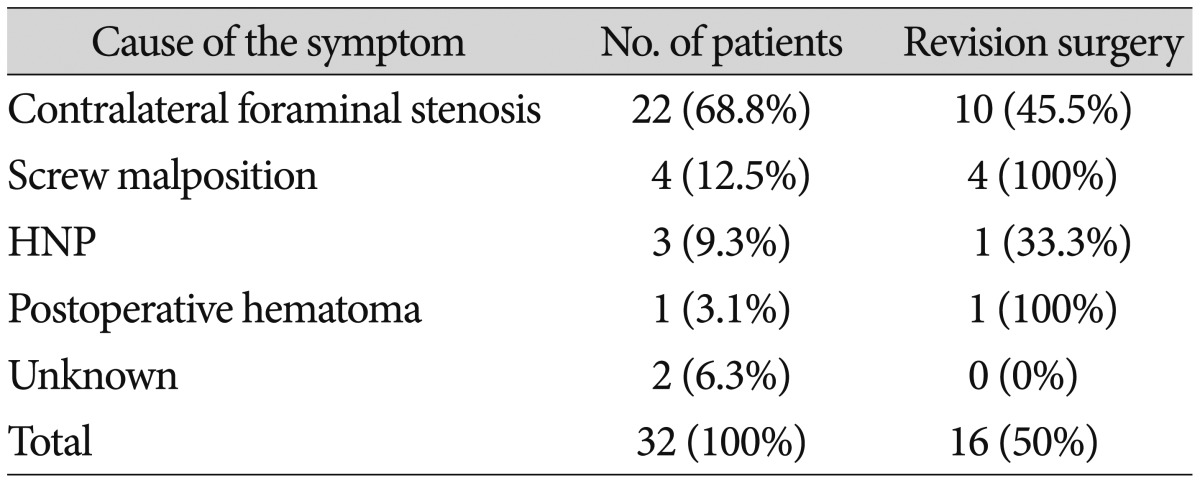
Causes of contralateral symptoms
The most common cause was contralateral foraminal stenosis (22 patients, 68.8%), followed by screw malposition (4 patients, 12.5%), HNP (3 patients, 9.3%), hematoma (1 patients, 3.1%), and unknown origin (2 patients, 6.3%) (Table 2).
Revision surgery
Revision surgery was performed for 16 (50.0%) of the 32 patients in the symptomatic group. Revision surgery was performed for 10 cases of contralateral foraminal stenosis (45.5%), 4 cases of screw malposition (100%), 1 case of HNP (33.3%), and 1 case of hematoma (100%). The 2 cases of unknown origin were successfully treated with nerve block.
Radiological factors
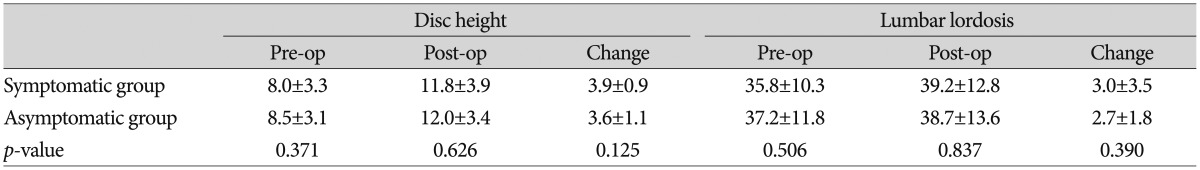
Pre- and postoperative disc heights were not different significantly between the two groups. The changes of disc height after surgery were similar in both groups (Table 3).
Preoperative LL's were 35.8±10.3° and 37.2±11.8°, and postoperative LL's were 39.2±12.8° and 38.7±13.6° in symptomatic and asymptomatic groups, respectively, showing no significant difference between the two groups. The change of LL was higher in symptomatic group (3.0±3.5°) than asymptomatic group (2.7±1.8°), but there was no statistical significance (Table 3).
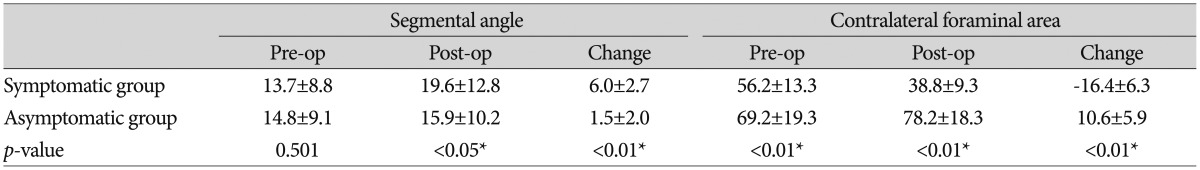
Pre- and postoperative SA's of asymptomatic group were 14.8±9.1° and 15.9±10.2°, which showed no significant difference between the two angles. On the contrary, pre- and postoperative SA's of symptomatic group were 13.7±8.8° and 19.6±12.8°, which showed a significant increase of the angle after surgery (p<0.05). The amount of change in SA's after surgery were 6.0±2.7° and 1.5±2.0° in symptomatic and asymptomatic groups, respectively, revealing a significantly large increase in symptomatic group (p<0.01) (Table 4). In conclusion, SA and change of SA were seem to be an important factor for occurrence of contralateral radiculopathy after unilateral TLIF, whereas LA was not.
Preoperative contralateral FA value of symptomatic group (56.2±13.3 mm2) was significantly smaller than that of asymptomatic group (69.2±19.3 mm2) (p<0.01). Postoperative contralateral FA's were 38.8±9.3 mm2 and 78.2±18.3 mm2 in symptomatic and asymptomatic groups, indicating marked decrease in the symptomatic group (p<0.01). Furthermore, postoperative changes of FA were -16.4±6.3 mm2 and 10.6±5.9 mm2 in symptomatic and asymptomatic groups, showing significant increase of the area after surgery in symptomatic group (p<0.01) (Table 4).
Clinical outcomes
Preoperative VAS scores were 5.8±3.2 and 6.0±2.9 in symptomatic and asymptomatic groups, and VAS scores at 3 months after surgery were 1.8±1.1 and 1.6±1.2, respectively, without significant difference between the two groups (Table 4). Preoperative ODI's were 66.8±21.7% and 61.0±23.5% in symptomatic and asymptomatic groups, and ODI's at 3 months after surgery were 18.6±10.5% and 20.2±12.8%, respectively, showing no significant difference between the two groups (Table 5).
DISCUSSION
TLIF operation has been widely used due to its excellent surgical outcome, relatively few complications, and high fusion rate112226). Additionally, the TLIF technique can preserves normal structures such as the facet joint and muscles at the contralateral side by using the unilateral approach4111529).
Contralateral radiculopathy after a unilateral TLIF is a complication spine surgeons often encounter1920). Although its causes have been studied through case reports, to our best knowledge, there has been no detailed study analyzing the cause. The incidence of contralateral radiculopathy after a unilateral TLIF was 5.9% based on our results. It seems to be closely related with contralateral foraminal stenosis, newly developed HNP, screw malposition, hematoma, among which contralateral foraminal stenosis was the most common cause. The contralateral complication itself didn't seem to affect the clinical results, which, we think, might be related with early diagnosis and proper management.
Although there have been many studies on various postoperative complications of lumbar spinal surgery through a number of literatures1561027), there have been no study on the incidence of contralateral radiculopathy after a unilateral TLIF. Thus, it is difficult to directly compare the degree of incidence shown in this study. However, the incidence rate of 5.9% is not likely to be small, considering the high frequency of TLIF use28). The reasons of unexpectedly high incidence seem to be the sporadic development of the complication, mild and transient symptom which can be controlled well with conservative management. So, it seems that we considered indiscreetly or ignored the complication. Therefore, the postoperative contralateral radiculopathy seems to be an important complication of unilateral TLIF surgeons should be cautious in the sense of not only its high incidence but also its unpredictability. So, analyzing its causes might be helpful in reducing or sometimes predicting the complication in the future.
Neural foramen decompression during TLIF operation is crucial for improving radiculopathy2032). Hunt et al.19) indicated contralateral foraminal stenosis after a unilateral TLIF might be the cause of contralateral symptoms. But their report didn't seem to have an objective evidence because of a lack of quantitative analysis with a large number of cases. We were able to confirm the causes in a relatively objective manner by analyzing various factors in a large number of patients in this study.
Iwata et al.20) reported the morphological change in the contralateral lumbar foramen after surgery in 58 patients who underwent unilateral TLIF. They proved the contralateral foraminal size was significantly increased with unilateral TLIF, which showed the possibility of indirect decompression of the contralateral side by unilateral insertion of a single cage. However, they reported that contralateral decompression was not highly effective when preoperative contralateral foraminal stenosis was present. This is comparable with the previous report of Hunt et al.19) that preexisting foraminal stenosis on the contralateral side might be the cause of contralateral symptoms. In our study, the contralateral foraminal area was already significantly smaller preoperatively and its size decreased significantly after surgery in the patients of symptomatic group. It seems to be ideal that establishing proper indications of unilateral or bilateral TLIF according to contralateral foraminal size, which must be investigated in the future study.
Appropriate restoration of lordosis during lumbar spine surgery is important for improving clinical outcomes and preventing failed back surgery syndrome with an iatrogenic flat back7916213031). On the other hand, increase in segmental lordotic angle of the operative level can cause contralateral foraminal stenosis1920). Our study showed similar results, both postoperative segmental angle and its change after surgery at the index level were found to be significant risk factors for contralateral radiculopathy after unilateral TLIF. However, the lordotic angle of whole lumbar spine did not have any effect on postoperative contralateral symptoms. Therefore, it seems that contralateral foraminal decompression or inserting bilateral cages might be safer when increase of segmental lordosis by surgery is predicted especially in the patients who already have narrow contralateral foramen preoperatively.
Lumbar foraminal stenosis can be caused by superior and ventral subluxations of the superior articular process of the inferior vertebra1324). The same changes were also observed in some of our patients of symptomatic group (Fig. 2). The superior or ventral displacement of superior articular process in the neural foramen seem to be related with inappropriately high grade rod compression at the contralateral side after the cage insertion or inappropriately high grade lordosis at the index level, respectively. The effect of superior articular process subluxation on the postoperative contralateral foraminal stenosis must be greater in the patients whose contralateral foraminal area was already smaller preoperatively. So, the size and insertion angle of cage seem to be risk factors for contralateral foraminal stenosis after unilateral TLIF. The curved cage was reported to be superior to the straight cage for making lumbar segmental angle23). But we used the straight cage for all cases in this study because of surgeons' preference. So, further study probing the mechanism or risk factors of contralateral foraminal stenosis related with cage seems to be necessary in the future.

Cases of contralateral radiculopathy after unilateral TLIF. A : Contralateral foraminal stenosis after surgery, showing superior and ventral subluxation of the superior articular process of inferior vertebra. B : Contralateral screw malposition. C : Newly developed HNP at the contralateral side. D : Epidural hematoma. TLIF : transforaminal lumbar interbody fusion, HNP : herniated nucleus pulposus.
It was difficult to understand the mechanism of the newly developed HNP contralateral to the operation side at first. But we now are understanding that the unilaterally inserted cage might push the disc material to the contralateral side and result in contralateral disc herniation. It seems to be related with the insufficient disc removal remaining large amount of disc material in the disc space.
Because this was conducted as a retrospective study, a prospective study will be needed in the future for a controlled study on more diverse factors. Although we were able to find several causes by analyzing various factors before and after surgery, we believe that there must be more risk factors which occur during surgery. CT was mainly used as a postoperative examination to avoid MRI artifacts caused by screw and rod. However, the disadvantage was that changes in soft tissues such as ligament and annulus in the foramen were not able to be counted properly by CT. The preoperative contralateral neural foraminal size seems to be an important risk factor, but unfortunately we did not assess the critical foraminal size which may provoke contralateral symptom after surgery.
The contralateral symptoms after unilateral TLIF may be reduced by being cautious to the risk factors. But we think another surgical techniques : bilateral TLIF, bilateral decompression with unilateral TLIF, should be needed to prevent the complication.
CONCLUSION
Postoperative contralateral radiculopathy is a complication of unilateral TLIF which can be caused by contralateral foraminal stenosis, screw malposition, newly developed HNP, and hematoma. The contralateral foraminal stenosis seems to be related with preoperative foraminal stenosis and postoperative increase of segmental angle. Considering its relatively high incidence and unpredictability, finding risk factors and mechanisms will be helpful to prevent or solve the problem.
Acknowledgements
This work was supported by the Technology Innovation Program (ATC; Advanced Technology Center, 10048523, Development of fluorography system under 50% irradiation dose with image quality on par with angiographic equipment to global leader in next generation) funded By the Ministry of Trade, industry & Energy (MI, Korea).