The Effects of Spinopelvic Parameters and Paraspinal Muscle Degeneration on S1 Screw Loosening
Article information
Abstract
Objective
To investigate risk factors for S1 screw loosening after lumbosacral fusion, including spinopelvic parameters and paraspinal muscles.
Methods
We studied with 156 patients with degenerative lumbar disease who underwent lumbosacral interbody fusion and pedicle screw fixation including the level of L5-S1 between 2005 and 2012. The patients were divided into loosening and non-loosening groups. Screw loosening was defined as a halo sign larger than 1 mm around a screw. We checked cross sectional area of paraspinal muscles, mean signal intensity of the muscles on T2 weight MRI as a degree of fatty degeneration, spinopelvic parameters, bone mineral density, number of fusion level, and the characteristic of S1 screw.
Results
Twenty seven patients showed S1 screw loosening, which is 24.4% of total. The mean duration for S1 screw loosening was 7.3±4.1 months after surgery. Statistically significant risk factors were increased age, poor BMD, 3 or more fusion levels (p<0.05). Among spinopelvic parameters, a high pelvic incidence (p<0.01), a greater difference between pelvic incidence and lumbar lordotic angle preoperatively (p<0.01) and postoperatively (p<0.05). Smaller cross-sectional area and high T2 signal intensity in both multifidus and erector spinae muscles were also significant muscular risk factors (p<0.05). Small converging angle (p<0.001) and short intraosseous length (p<0.05) of S1 screw were significant screw related risk factors (p<0.05).
Conclusion
In addition to well known risk factors, spinopelvic parameters and the degeneration of paraspinal muscles also showed significant effects on the S1 screw loosening.
INTRODUCTION
Many studies have reported frequent nonunion in the lumbosacral segment comparing to other levels289) and frequent sacral pedicle screw loosening in the cases of long level lumbosacral fusion181924). The sacral screw loosening was reported to be occurred in about 15.6-41.9%101634). Iliac screw, bicortical screw insertion, and cement augmentation have been attempted as preventative measures according to known risk factors related with techniques for S1 screw and bone quality12729303336374448). Recently, spinal balance and paraspinal muscles are known to be closely related with hardware failure especially after long level fixation for spinal deformity525). In other words, spinal balance and paraspinal muscles may have effects on the mechanical stress or mechanical failure of S1 screw. However, to the best of our knowledge, there was no report studying their relationships directly.
In this study, we tried to investigate various risk factors for S1 screw loosening after lumbosacral fusion, including spinopelvic parameters and the degenerative changes of paraspinal muscles.
MATERIALS AND METHODS
Patients
Total 196 patients underwent spinal fusion operations including L5-S1 level for degenerative lumbar diseases between 2005 and 2012 in our hospital. All the enrolled patients were followed up for more than 24 months after surgery. Seven cases of revision surgery, a known risk factor for screw loosening5), were excluded from this study. Thirty-three patients received open pedicle screw fixation were also excluded. Finally, we conducted this study with 156 patients with 68 males and 88 females. The mean age at the time of surgery was 58.0±12.7 years. They were divided into two groups, loosening group with S1 screw loosening and non-loosening group without S1 screw loosening at 1 year after surgery.
Preoperative diagnosis consisted of spinal stenosis in 144, spondylolisthesis in 100, degenerative scoliosis in 4, and discogenic pain in 2. There was no patient with sagittal imbalance on whole spine radiographic exam. All the patients received transforaminal lumbar interbody fusion (TLIF) with unilateral single interbody cage filled with autologous bone chips obtained from laminectomy and facetectomy. Numbers of fusion levels were 1-4 levels. Two percutaneous pedicle screw systems (Sextant and Longitude Systems; Medtronics, Memphis, TN, USA) were used for fixation. The diameter of S1 screw ranged 6.0-8.5 mm, and the length 35-50 mm. Screw loosening was defined as a halo sign showing a radiolucent line of ≥1 mm around the screw639) was found with simple radiographic films in one or both sides during 1 year after the surgery (Fig. 1).
Risk factors and radiological evaluation
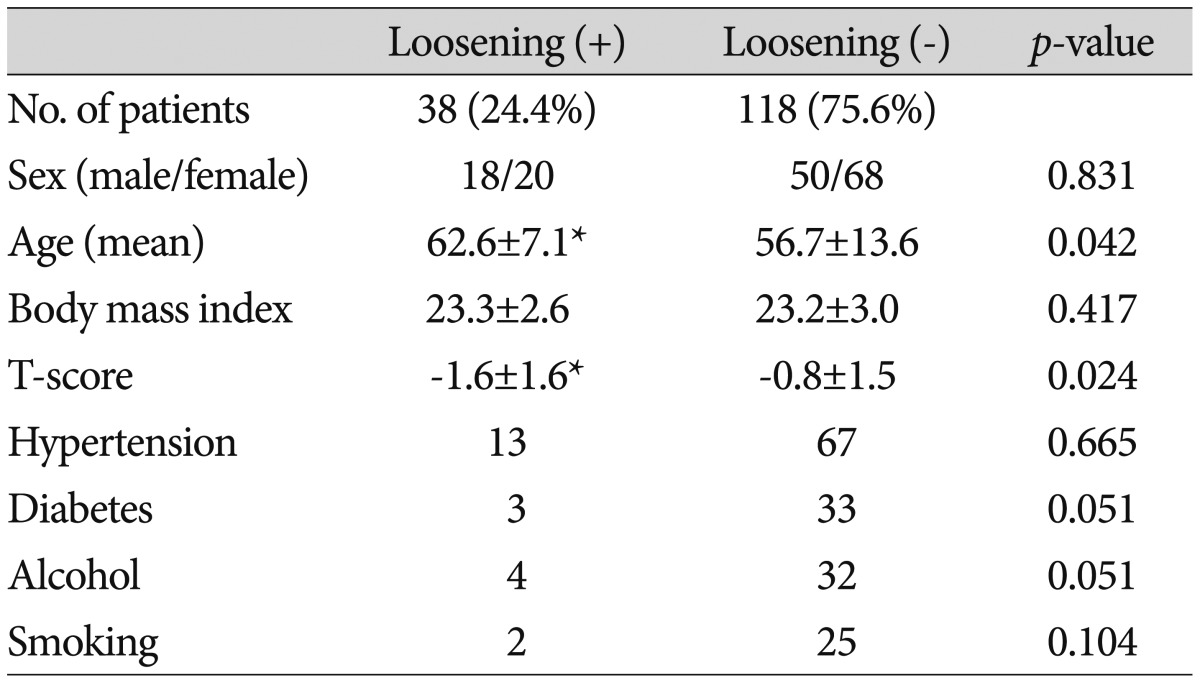
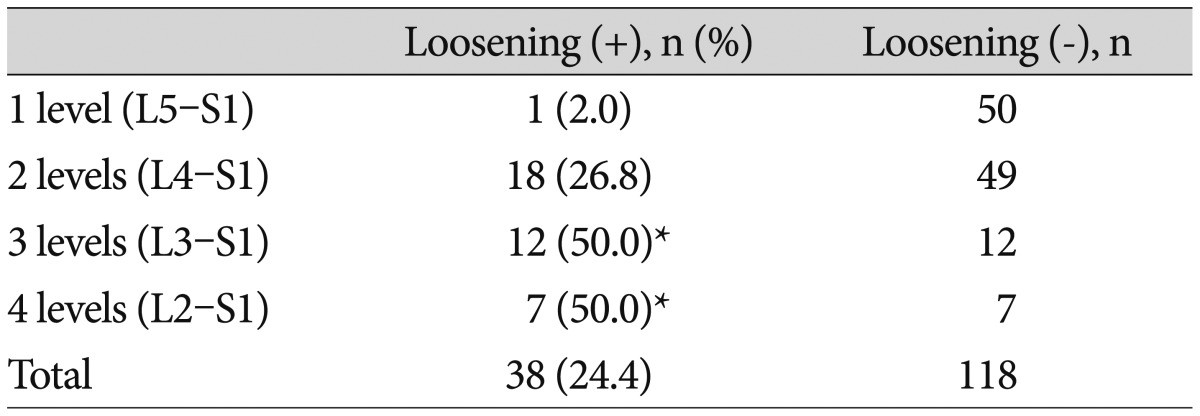
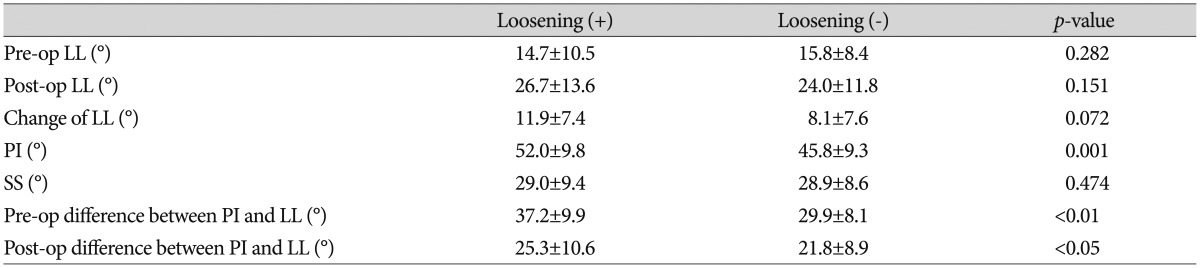
Patient's factors, sex, age, body mass index (BMI), bone mineral density (BMD), hypertension, diabetes, alcohol, and smoking, were checked (Table 1). Numbers of fusion levels were 1 (L5-S1), 2 (L4-S1), 3 (L3-S1), and 4 (L2-S1) levels (Table 2). T-score of lumbar spine was checked by measuring BMD with dual-energy radiograph absorptiometry (Lunar Prodigy; General Electric, Madison, WI, USA). Spinopelvic parameters, pre- and postoperative lumbar lordosis (LL), pelvic incidence (PI), sacral slope (SS), and difference between PI and LL (PI-LL) were measured with whole spine radiographic exam. As muscle related factors, cross sectional area (CSA) and mean signal intensity of paraspinal muscles were checked preoperatively at L5-S1 disc level with T2 weighted MRI axial images (Fig. 2). Axial and sagittal angles, diameter, length, and intraosseous length of S1 screws were checked with postoperative CT as screw related factors (Fig. 3).
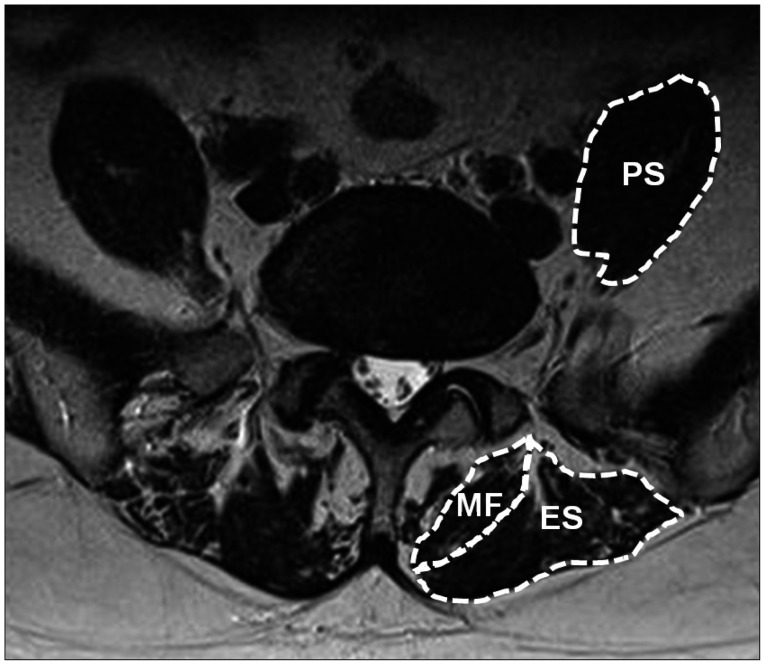
Paraspinal muscles at L5-S1 level, multifidus muscle (MF), erector spinae muscle (ES), and psoas muscle (PS).

A : Sagittal angle of S1 screw between screw and upper end plate of S1 vertebra on simple lateral radiograph. B : Axial angle of S1 screw between screw and vertical line (a) and intraosseous length of S1 screw as the length of intraosseous portion of the screw on postoperative CT (b).
Muscle factors were measured for 3 paraspinal muscle groups, multifidus, erector spinae, and psoas muscles. The erector spinae muscles include both longissimus muscle and iliocostalis muscles at L5-S1 level. The signal intensity of muscle on T2 weighted MRI mainly reflects the amount of intramuscular fat content which is known to be related with muscle degeneration1317). The cross sectional area and mean signal intensity of the muscle groups were measured with tools of PACS software (M-view, Infinitt Healthcare, Seoul, Korea). All the spinopelvic parameters, muscle factors, and screw factors were measured 2 times, and their mean values were used for analysis. The screw related factors were checked at both sides separately, and the total number of measured S1 screws was 268. All the data of screw factors in the loosening group were unexceptionally those of the loosened screws because all the patients in the group showed screw loosening bilaterally.
The sagittal angle of S1 screw was measured as the angle formed between S1 screw and S1 upper plate on simple lateral radiograph. The axial angle of S1 screw was measured as the angle between S1 screw and vertical line. The intraosseous length of S1 screw was measured as the length of intraosseous portion of the screw at S1 vertebra on postoperative CT.
To assess reliability of measurements, two authors measure the radiological parameters for 2 times with 2 weeks interval between the measurements. Statistical analysis was done with Student t-test, chi-square test, and Pearson's correlation coefficient. A p value less than 0.05 was considered to be statistically significant. The intraobserver and interobserver intraclass correlation coefficients (ICC) were calculated for LL, PI, SS, CSA and mean signal intensity of paraspinal muscles, angles (axial and sagittal angles) and intraosseous length of S1 screw.
RESULTS
S1 screw loosening occurred in 38 of total 156 patients (24.4%). Mean age was significantly higher in loosening group (62.6±7.1) than non-loosening group (56.7±13.6) (p<0.05). The mean T-scores of BMD was significantly lower in loosening group (-1.6±1.6) than non-loosening group (-0.8±1.5) (p<0.05). There was no significant difference in gender, BMI, hypertension, diabetes, alcohol, and smoking history between the two groups (Table 1).
The mean duration for detection of screw loosening was 7.3±4.1 (2-15) months. The rate of S1 screw loosening according to the number of fusion levels were 2.0%, 26.8%, 50.0%, and 50.0% in 1, 2, 3, and 4 levels fusion groups. The rate of S1 screw loosening showed a significantly higher rate in 3 or 4 levels fusion comparing to 1 level fusion (p<0.05) (Table 2).
Mean pre- and postoperative LL values were 14.7±10.5° and 26.7±13.6° in the SL group, and 15.8±8.4° and 24.0±11.8° in the non SL group. Sacral slope angles were 29.0±9.4° and 28.9±8.6° in the loosening and non-loosening groups, respectively. The sacral slope, pre- and postoperative LL angles were not different between the two groups (Table 3). The change of LL angle after surgery was greater in the loosening group (11.9±7.4°) than and non-loosening group (8.1±7.6°), but there was no statistical significance (Table 3). Mean PI was significantly higher in the loosening group (52.0±9.8°) than those of non-loosening group (45.8±9.3°) (p<0.01) (Table 3). Pre- and postoperative PI-LL's were significantly greater, 37.2±9.9° (p<0.01) and 25.3±10.6° (p<0.05), in loosening group, comparing to those of non-loosening group, 29.9±8.1° and 21.8±8.9° (Table 3). The intraobserver ICC's were 0.97, 0.90, and 0.96 in LL, PI, and SS, respectively. The interobserver ICC's were 0.93, 0.84, and 0.94 in LL, PI, and SS, respectively.
Mean CSA's of multifidus muscle, erector spinae muscle, and psoas muscle, checked at L5-S1 disc level, were 380.7±251.5 mm2, 803.2±200.2 mm2, and 843.1±276.4 mm2 in loosening group, and 905.7±271.1 mm2, 674.4±150.4 mm2, and 911.5±264.6 mm2 in non-loosening group (Table 4). CSA's of multifidus muscle (p<0.05) and erector spinae muscle (p<0.001) were significantly smaller in loosening group than non-loosening group. Mean signal intensity values on T2 MRI of the respective muscles were 454.0±368.3, 436.6±350.2, and 134.2±92.8 in loosening group, and 355.6±166.9, 335.8±163.9, and 137.1±68.0 in non-loosening group. The muscular signal intensities of multifidus and erector spinae muscles were significantly higher in loosening group (p<0.05) (Table 4). But psoas muscle didn't show any difference in both CSA and signal intensity between the two groups. There was no significant correlation between significant spinopelvic parameters (PI and postoperative PI-LL) and the degenerative changes (CSA and mean signal intensity) of paraspinal muscles according to Pearson correlation coefficient (p>0.05) (Table 5). The intraobserver ICC's were 0.90, 0.93, and 0.97 in CSA's of MF, ES, and PS. The intraobserver ICC's were 0.95, 0.97, and 0.98 in mean signal intensity values of MF, ES, and PS. The interobserver ICC's were 0.85, 0.85, and 0.90 in CSA's of MF, ES, and PS. The interobserver ICC's were 0.91, 0.90, and 0.94 in mean signal intensity values of MF, ES, and PS.
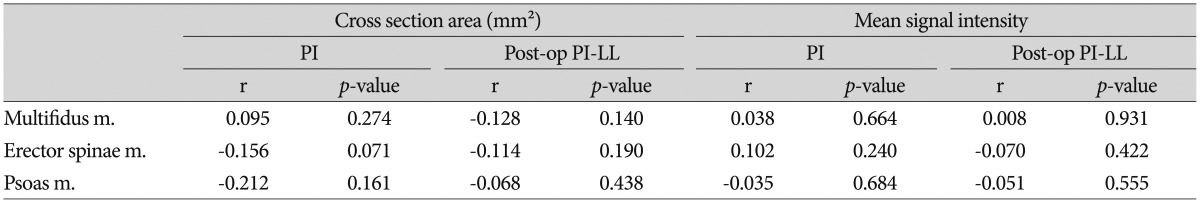
Pearson correlation coefficients between spinopelvic parameters and the degenerative changes of paraspinal muscles
The mean axial angle of S1 screw was 8.0±4.7° in loosening group, which was significantly lower than those of non-loosening group, 13.0±5.2° (p<0.001) (Table 6). Other screw related factors including sagittal angle, diameter, and length of S1 screw were similar between the two groups. Even though the whole length of S1 screw was not so meaningful, intraosseous length of S1 screw was significantly longer, 31.8±5.1 mm, in non-loosening group than loosening group, 29.5±3.7 mm (p<0.05) (Table 6). The intraobserver ICC's were 0.98, 0.95, and 0.90 in axial angle, sagittal angle, and intra-osseous length of S1 screw, respectively. The interobserver ICC's were 0.90, 0.88, and 0.85 in axial angle, sagittal angle, and intra-osseous length of S1 screw, respectively.
DISCUSSION
Among the patients underwent spinal fusion operation including S1, the loosening rate of S1 screw had been reported about 15.6-46.5%101634). Screw loosening rate of lumbar spine was reported to be about 10-20%, which is, in general, lower than S1 screw loosening rate45). There is a tendency of decreased fusion rate at lumbosacral level due to increased pseudoarthrosis435). In our study, S1 screw loosening occurred in 24.4%, which was relatively high level comparable with other reports.
This is because the sacrum is composed primarily of cancellous bone, and receives a greater mechanical load than other segments28). The anatomical characteristics of the S1 pedicle, a larger diameter and shorter length than lumbar pedicles, indicate that S1 screw loosening occurs more frequently due to the structural weakness of the S1 body and pedicle31). Other factors that reportedly contribute to sacral screw failure include inappropriate direction or depth of screw insertion, and large cantilever bending moments loaded by long level instrumentation23443). In relation to the fusion length there was no specified criteria for the use of S1 protective procedures according to the number of fusion levels. Our data showed 3 or more levels (L3-S1 or L2-S1) significantly increased the risk of the S1 screw loosening, which seemed to suggest the need for use of S1 protective procedures in the cases with 3 or more fusion levels.
There have been various techniques for the protection of S1 screw including sacropelvic fixation130374448), bicortical or tricortical insertion of S1 screw2729), and cement augmentation3336). We also used these techniques as preventive methods in selected patients with high risk of screw loosening, osteoporosis or old age, which were proved as risk factors for the S1 screw loosening, who were not enrolled in this study. Although the techniques must have a strong preventive effect for S1 screw loosening, we could not analyze their effects because of their selective use for high risk patients.
Differences in fusion methods also appear to influence screw loosening. Some reports indicated TLIF showed a lower screw loosening rate than posterior lumbar interbody fusion (PLIF)1447). Xu et al.46) reported the mechanical difference between TLIF and PLIF by proving the difference in screw stress, which might be related with increased possibility of S1 screw loosening. However, we could not find a study directly reporting S1 screw loosening after TLIF operation. Considering the different biomechanical effect on pedicle screw between TLIF and PLIF, a separate study on risk factors of S1 screw loosening for both types of fusion seems to be necessary. In this study, we selected patients underwent TLIF for investigation of S1 screw loosening.
The importance of surgical recovery of lumbar lordosis has been reported in many papers, and insufficient lumbar lordotic angle seem to be associated with lower back pain and functional loss202223). During spinal fusion, it is more important to correct lumbar lordotic angle within its physiological range, usually greater than PI1640). Accordingly, larger preoperative PI demands greater lumbar lordotic angle during surgery40). Decreased lordotic angle can cause increased load to the adjacent segments712). According to our data, the preoperative PI, difference between PI and lumbar lordotic angle was significantly greater in the screw loosening group comparing to the non-loosening group. When the patients had high preoperative PI-LL difference, 37.2±9.9°, the risk S1 screw loosening increased significantly. This insufficient correction of a lordotic angle, still high postoperative PI-LL difference, 25.3±10.6°, seems to increase the risk of S1 screw loosening due to more bending moment and mechanical stress to the screw. Both pre- and postoperative PI-LL's seem to be important risk factors. But we think the postoperative PI-LL is a more important factor because it can be reduced by surgery.
Paraspinal muscles play an important role in maintaining segmental, regional, and global stability25). The indicators of degenerative change in the paraspinal muscles include cross-sectional area and fatty changes. Degeneration in the cross-sectional area appears as muscle atrophy1526); fatty changes in muscles are also a form of degeneration, which is closely associated with functional decrease11263241). Lee et al.25) indicated that the fat content of the paraspinal muscles was the factor with the greatest influence on the result of lumbosacral fusion operation. According to our results, smaller cross-sectional areas and greater fatty changes in multifidus and erector spinae muscles may affect clinical result of fusion operation by way of increasing S1 screw loosening.
The spinopelvic parameters with significant effect on S1 screw loosening, PI and postoperative PI-LL, were selected to test correlation with muscular degenerative indices, CSA and mean signal intensity. But, there was no significant correlation between the spinopelvic parameters and degenerative indices of paraspinal muscles. This suggests the two types of risk factors, spinopelvic parameters and muscular degeneration, may have their own effects on S1 screw loosening and can have synergistic effect. We didn't analyze their synergistic effect, it seems to need further study investigating their independency or synergistic effect on the development of S1 screw loosening.
Screw angulation strengthens the resistance to straight pullout. Many studies have shown that two angulated screws have greater resistance to pullout than parallel ones3384249). Krag et al.21) performed biomechanical testing on pedicle screws, and indicated that angulated screws are stronger due to a 'toe nail' effect. Our results also confirmed that the S1 screw axial angle, not the sagittal angle, was important to protect S1 screw. In addition, the long intraosseous length of screw, not the diameter or whole length of screw, was noted to reduce the risk of S1 screw loosening significantly.
A retrospective study with a small number of patients was a limitation of our study. Although a study on sacropelvic parameters was conducted, a direct relationship with sagittal balance was not fully investigated because our study didn't enroll any patient with sagittal imbalance. The data of cross sectional area and fatty degeneration of paraspinal muscles could not explain actual muscle function. Moreover, our data were based on radiological findings, which did not reflect clinical outcomes directly. Therefore, additional studies related to these subjects are deemed to be necessary in the future.
CONCLUSION
Most of the risk factors for S1 screw loosening, including age, osteoporosis, number of fusion levels, toe nail effect of screw, were proved to be related with S1 screw loosening, which were comparable with other reports. But we focused on the additional two types of possible risk factors, spinopelvic parameters and back muscle degeneration. The high PI and high PI-LL were proved to be significant risk factors, suggesting the importance of making sagittal balance during surgery. Back muscle weakness represented by CSA and fat degeneration was also proved to be a risk factor, which shows the importance of preoperative evaluation for paraspinal muscles and postoperative back muscle rehabilitation program.