Correction of Spondylolisthesis by Lateral Lumbar Interbody Fusion Compared with Transforaminal Lumbar Interbody Fusion at L4–5
Article information
Abstract
Objective
In an aging society, the number of patients with symptomatic degenerative spondylolisthesis (DS) is increasing and there is an emerging need for fusion surgery. However, few studies have compared transforaminal lumbar interbody fusion (TLIF) and lateral lumbar interbody fusion (LLIF) for the treatment of patients with DS. The purpose of this study was to investigate the clinical and radiological outcomes between TLIF and LLIF in DS.
Methods
We enrolled patients with symptomatic DS at L4–5 who underwent TLIF with open pedicle screw fixation (TLIF group, n=41) or minimally invasive LLIF with percutaneous pedicle screw fixation (LLIF group, n=39) and were followed-up for more than one year. Clinical (visual analog scale and Oswestry disability index) and radiological outcomes (spondylolisthesis rate, segmental sagittal angle [SSA], mean disc height [MDH], intervertebral foramen height [FH], cage subsidence, and fusion rate) were assessed. And we assessed the changes in radiological parameters between the postoperative and the last follow-up periods.
Results
Preoperative radiological parameters were not significantly different between the two groups. LLIF was significantly superior to TLIF in immediate postoperative radiological results, including reduction of spondylolisthesis rate (3.8% and 7.2%), increase in MDH (13.9 mm and 10.3 mm) and FH (21.9 mm and 19.4 mm), and correction of SSA (18.9° and 15.6°) (p<0.01), and the changes were more stable from the postoperative period to the last follow-up (p<0.01). Cage subsidence was observed significantly less in LLIF (n=6) than TLIF (n=21). Fusion rate was not different between the two groups. The clinical outcomes did not differ significantly at any time point between the two groups. Complications were not statistically significant. However, TLIF showed chronic mechanical problems with screw loosening in four patients and LLIF showed temporary symptoms associated with the surgical approach, such as psoas and ileus muscle symptoms in three and two cases, respectively.
Conclusion
LLIF was more effective than TLIF for spondylolisthesis reduction, likely due to the higher profile cage and ligamentotactic effect. In addition, LLIF showed mechanical stability of the reduction level by using a cage with a larger footprint. Therefore, LLIF should be considered a surgical option before TLIF for patients with unstable DS.
INTRODUCTION
Degenerative spondylolisthesis (DS) is defined as the forward slippage of an upper vertebra with respect to a lower vertebra, which causes back pain or radiculopathy due to spinal canal stenosis or foraminal stenosis [11]. DS occurs mainly in those above 50 years of age and about 73% of cases occur at the L4–5 level. The reported prevalence is 2.7% in men and 8.1% in women [16]. In particular, the prevalence of spondylolisthesis in the Chinese population over 65 years is 19.1% in men and 25.0% in women, and spondylolisthesis progression and de novo spondylolisthesis occur in more than 12% of both men and women [13,29]. A recent study on patients with symptomatic DS reported that patients who received surgery had significantly greater improvements in pain and function compared to those two received non-operative treatment in eight years of follow-up [1]. Therefore, surgery is an important treatment in patients with symptomatic DS.
Among the surgical treatments for patients with symptomatic DS, intervertebral fusion is the main surgical method used to stabilize the spine and reduce pain and disability; its types include the posterolateral (posterior lumbar interbody fusion and transforaminal lumbar interbody fusion [TLIF]), lateral (lateral lumbar interbody fusion [LLIF], direct lateral interbody fusion [DLIF], extreme lateral interbody fusion [XLIF], and oblique lateral interbody fusion [OLIF]), and anterior (anterior lumbar interbody fusion) approaches [9,18,24]. LLIF is a relatively new minimally invasive surgery (MIS) for the treatment of DS and has the advantage of being able to insert an interbody cage with a large foot-print without injury to posterior facets [6]. While recent findings on the treatment of DS with LLIF have been reported and comparative studies of LLIF with other therapies have been published, there remains controversy regarding whether LLIF is the optimal treatment for DS [5,10,15,18,22,23,25,30]. In addition, direct comparison studies between TLIF and MIS-LLIF were not only small in number but also insufficient for explaining the recent advances of MIS-LLIF [15,25].
We compared the clinical and radiological outcomes of TLIF and MIS-LLIF (DLIF or OLIF), which have mainly performed for DS in our hospital, to investigate better fusion surgery for patients with symptomatic DS, whose numbers are increasing in aging societies.
MATERIALS AND METHODS
This study was a single-center study in which the surgeries were conducted by two neurosurgeons (Y.B.K. and S.W.P.). TLIF was performed only by Y.B.K. and LLIF was performed only by S.W.P. We retrospectively reviewed and enrolled patients with symptomatic DS who underwent TLIF (TLIF group) or MIS-LLIF (LLIF group) at the L4–5 level between January 2011 and December 2015 and were followed-up for more than one year. Age, sex, bone marrow density, and body mass index were evaluated. This study was reviewed and approved by the Institutional Review Board (CAUH IRB No. 1806-002-16175).
Surgical techniques
The TLIF group underwent unilateral open TLIF with a single capstone cage (Medtronic, Minneapolis, MN, USA) filled with autologous bone. The pedicle screw fixation (Zenius system, Medyssey, Jecheon, Korea) was done by a conventional open technique ipsilaterally and an interfascial approach contralaterally. All components for central stenosis and foraminal stenosis were decompressed directly during the TLIF approach.
The LLIF group un derwent MIS-DLIF or OLIF by using a transpsoas or extrapsoas retroperitoneal ap proach and percutaneous pedicle screw fixation. The LLIF group was treated by using a Clydesdale cage (Medtronic, Memphis, TN, USA) filled with a demineralized bone matrix (DBM, Grafton; Medtronic, Minneapolis) and a percutaneous pedicle screw fixation system (Longitude II system, Medtronic, Memphis). All foraminal stenosis (23 of 39 patients) were decompressed indirectly by increasing the disc height and correcting the spondylolisthesis. Additional posterior decompression was performed for pa tients in the LLIF group (16 of 39 patients) with severe central stenosis.
Clinical evaluation
We assessed the clinical outcomes by using the visual analog scale (VAS) for back pain (VAS-back) and leg pain (VASleg), as well as the Oswestry disability index (ODI). VAS and ODI were evaluated preoperatively (PreVAS and PreODI) and one year postoperatively (PostVAS and PostODI). In addition, we also assessed postoperative complications, the length of hospital stay, and operation time.
Radiographic measurement
We checked the spondylolisthesis rate, segmental sagittal angle (SSA), mean disc height (MDH), intervertebral foramen height (FH), and cage subsidence by simple radiographs. In addition, lumbar lordosis (LL) was measured by 36-inch whole-spine X-ray films.
The spondylolisthesis rate (%) was calculated by dividing the amount of L4 body displacement on the L5 upper endplate by the anterior-posterior diameter of the L5 upper endplate. The SSA was measured as the angle between the superior endplate of the L4 vertebra and the inferior endplate of the L5 vertebra. The MDH was calculated as the mean value of the anterior and posterior disc heights (mm) in lateral images. The FH was measured as the distance between the inferior margin of the L4 pedicle and the superior margin of the L5 pedicle in the lateral view. The LL was measured as the angle between the superior endplates of L1 and S1. Cage subsidence was defined as when a cage sank into adjacent vertebral body more than 2 mm on the last follow-up (f/u) lateral image.
Fusion rate was evaluated by two methods. First, grade of 1 or 2 on plain radiography was defined as a successful bony fusion by using Bridwell-Lenke grading system (grade 1 : completely remodeled with trabeculae across the disc space; grade 2 : graft intact with no lucent lines between the graft and adjacent endplates; grade 3 : graft intact but with a radiolucent line between the graft and an adjacent endplate; and grade 4 : lucency along the entire border of the graft or lucency around a pedicle screw or subsidence of the graft) [4]. Second, grade of 1 or 2 on computed tomography (CT) imaging at 1-year postoperative (1 YA) was defined as a successful bony fusion by using CT-based classification (grade I : complete fusion, implies cortical union of the allograft and central trabecular continuity; grade II : partial fusion, implies cortical union of the structural allograft with partial trabecular incorporation; grade III : unipolar pseudarthrosis, denotes superior or inferior cortical non-union of the central allograft with partial trabecular discontinuity centrally; and grade IV : bipolar pseudarthrosis, suggests both superior and inferior cortical nonunion with a complete lack of central trabecular continuity) [27].
The radiologic parameters were evaluated at preoperative (Preop), immediate postoperative (Postop), 1 YA, and last f/u. All radiologic measurements were made using the measuring tool within the picture archiving communication system in Chung-Ang Univertisy Hospital. Two observations were made at an interval of at least one week by two neurosurgeons (M.J.K. and S.W.P.), and the mean values were used for the study. The intraclass correlation coefficient (ICC) was checked to verify the intra-observer and inter-observer reliability of the radiologic measurements.
Statistical analysis
The radiological and clinical outcomes were compared in each group using paired t-tests. The outcomes between the DLIF and OLIF groups were compared using Student’s t- and chi-square tests. p-values <0.05 were considered statistically significant. The ICC values were graded using previously described semiquantitative criteria (excellent for values in the 0.90–1.0 range, good for 0.70–0.89, fair/moderate for 0.50– 0.69, low for 0.25–0.49, and poor for 0.0–0.24).
RESULTS
Baseline characteristics
There were 41 (male : female=9 : 32) and 39 (male : female=11 : 28) patients in the groups, respectively. In these groups, 34 and 28 and seven and 11 patients had grade I and II spondylolisthesis, respectively. The mean follow-up period was 27.2±18.0 and 33.6± 15.9 months in the TLIF and LLIF groups, respectively. The baseline characteristics are described in Table 1, and there were no significant differences between the TLIF and LLIF groups.
Clinical outcomes
In the TLIF and LLIF groups, the PreVAS-back were 7.6±1.4 and 7.5±1.5, the PreVAS-leg were 6.0±1.5 and 6.6±2.0, and the PreODI were 44.5±11.7 and 45.6±12.6%, respectively. The PostVAS-back were 2.2±1.3 and 1.9±0.6, the PostVAS-leg were 1.8±0.8 and 1.6±0.7, and the PostODI were 18.0±5.9 and 16.5± 6.4%, respectively. In both groups, both PostVAS and PostODI showed a significant improvement compared to the preoperative values (p<0.001), and there were no significant differences between the two groups (Table 2).
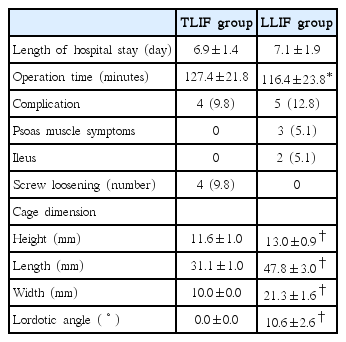
Cage dimensions
The cage height, length, width, and angle were 11.6±1.0 mm, 31.1±1.0 mm, 10.0±0.0 mm, and 0.0±0.0˚ in the TLIF group, respectively, and 13.0±0.9 mm, 47.8±3.0 mm, 21.3±1.6 mm, and 10.6±2.6˚ in the LLIF group, respectively. The cages in the LLIF group were significantly taller, longer, wider, and had larger angles than those in the TLIF group (p<0.001) (Table 3).
Perioperative parameters
The mean hospital stays were 6.9±1.4 and 7.1±1.9 days in the TLIF and LLIF groups, respectively and there was no significant difference. The mean operation times were 127.4±21.8 and 116.4±23.8 minutes in the TLIF and LLIF groups, respectively, and the LLIF group had a significantly shorter operation time than that in the TLIF group (p=0.034).
The complications observed during follow-up included four instances of screws loosening (one reoperation) in the TLIF group and three psoas muscle symptoms and two postoperative ileus in the LLIF group. In the LLIF group, there were no instances of genitofemoral nerve symptoms, sympathetic symptom, or screw loosening and all complications improved within a few days. There was no surgical site infection or fatal complications in either group. The types of complications differed between groups, but the difference was not statistically significant (Table 3).
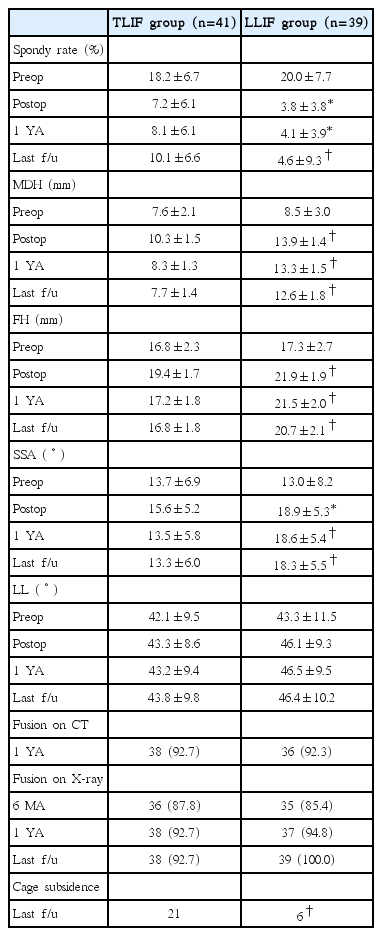
Radiographic parameters (Table 4)
There were no significant differences in Preop-spondylolisthesis rate, MDH, FH, SSA, and LL between the TLIF and LLIF groups.
The spondylolisthesis rate of Postop, 1 YA, and last f/u were 7.2 ±6.1, 8.1±6.1, and 10.1±6.6% in the TLIF group, respectively, and 3.8±3.8 (p=0.005), 4.1±3.9 (p=0.001), and 4.6±9.3% (p<0.001) in the LLIF group, respectively. The spondylolisthesis rates after surgery were significantly lower in the LLIF group than those in the TLIF group at all postoperative periods.
The MDH of Postop, 1 YA, and last f/u were 10.3±1.5, 8.3±1.3, and 7.7±1.4 mm in the TLIF group, respectively, and 13.9±1.4, 13.3±1.5, and 12.6±1.8 mm in the LLIF group, respectively. The MDH’s were significantly higher in the LLIF group than those in the TLIF group at all postoperative periods (p<0.001).
The FH of Postop, 1 YA, and last f/u were 19.4±1.7, 17.2±1.8, and 16.8±1.8 mm in the TLIF group, respectively, and 21.9± 1.9, 21.5±2.0, and 20.7±2.1 mm in the LLIF group, respectively. The FH’s were significantly higher in the LLIF group than those in the TLIF group at all postoperative periods (p<0.001). The SSA of Postop, 1 YA, and last f/u were 15.6±5.2, 13.5± 5.8, and 13.3±6.0˚ in the TLIF group, respectively, and 18.9±5.3 (p=0.007), 18.6±5.4 (p<0.001), and 18.3±5.5˚ (p<0.001) in the LLIF group, respectively. The SSA’s were significantly larger in the LLIF group than those in the TLIF group at all postoperative periods.
The LL of Postop, 1 YA, and last f/u were 43.3±8.6, 43.2±9.4, and 43.8±9.8˚ in the TLIF group, respectively, and 46.1±9.3, 46.1±9.5, and 46.4±10.2˚ in the LLIF group, respectively. There were no significant differences between the two groups.
The number of cage subsidence was 21 and six in the TLIF and LLIF groups, respectively, and cage subsidence was significantly less in LLIF group (p<0.001).
In the TLIF group, the mean difference between Postop and last f/u values for the spondylolisthesis rate, MDH, FH, and SSA were -2.9±3.9% (-63.8%), 2.6±1.3 mm (24.7%), 2.5±1.4 mm (13.2%), and 2.3±2.5˚ (17.4%), respectively. The corresponding values in the LLIF group were -0.8±1.5% (-16.2%), 1.3±1.0 mm (9.7%), 1.2±0.9 mm (5.5%), and -0.5±1.5˚ (2.9%), respectively, and the differences were significantly less than those in the TLIF group (Table 5).

Mean changes (Δ) of radiologic parameters between the immediate postoperative and the last follow-up values
The fusion rate on plain radiography was 87.8% and 85.4% at postoperative 6 months, 92.7% and 94.8% at 1 YA, and 92.7% and 100.0% at last f/u in TLIF and LLIF groups, respectively. The fusion rate on CT scan was 92.7% and 92.3% at 1 YA in the TLIF and LLIF groups, respectively, and there was no significant difference between the two groups on plain radiography and CT.
The intra- and inter-observer ICCs were 0.85–0.94 and 0.75–0.92, respectively (Table 6).
DISCUSSION
TLIF and LLIF use different mechanisms to decompress stenosis due to DS (direct vs. indirect decompression). TLIF provides a good visualization of the neural elements through direct decompression of the posterior element [8,12]. LLIF approaches the intervertebral disc space through retroperitoneal transpsoas (DLIF/XLIF) or extrapsoas (OLIF) and indirectly decompresses the spinal canal and intervertebral foramen by inserting a cage with large footprint [5,10,23].
Sembrano et al. [25] reported the clinical outcomes of TLIF and XLIF in patients with DS. They reported high mean improvements in pain (73% and 64% in back pain, 79% and 74% in leg pain), disability (53% and 57%), and quality of life (63% and 64%) in both the TLIF and XLIF groups, with no significant differences between the two groups. In our study, Post- VAS-back and PostVAS-leg were improved by 71.1% and 70% in the TLIF group, respectively, and by 74.7% and 75.8% in the LLIF group, respectively. In addition, PostODI was improved by 59.6% and 63.6% in the TLIF and LLIF groups, respectively. According to our results, TLIF and LLIF significantly improved pain and disability in patients with DS without significant differences between the two groups, similar to the results of previous studies [6,25].
A prospective study of radiological outcomes of TLIF and XLIF compared different mechanisms (direct vs. indirect), reporting that the average postoperative disc height was significantly higher in the XLIF group (10.1±2.1 mm) than that in the TLIF group (9.1±1.8 mm) and that the foraminal dimension was significantly larger in the XLIF group than that in the TLIF group [15]. In our study, both Postop-MDH and Postop- FH were significantly higher in the LLIF group (13.9±1.4 mm and 21.9±1.9 mm, respectively) than those in the TLIF group (10.3±1.5 mm and 19.4±1.7 mm, respectively); these results are similar to those of other studies [7,19,26]. These results indicate that LLIF is effective for indirect decompression by increasing disc height more than that with TLIF.
However, unlike a previous study [15], the Postop-MDH difference between the TLIF and LLIF groups was larger and the Postop-SSA was significantly larger in the LLIF group (18.9± 5.3˚) than that in the TLIF group (15.6±5.2˚) in our study. The differences between the two studies are likely due to differences in cage dimension, which is similar to the results of other studies [2,26]. In a previous study [15], the mean cage heights were 10.6 and 11.2 mm and the mean cage angles were 0˚ and 5.4˚ in the TLIF and XLIF groups, respectively. However, in our study, the mean cage heights were 11.6±1.0 and 13.0±0.9 mm and the mean cage angles were 0.0±0.0 and 10.6±2.6˚ in the TLIF and LLIF groups, respectively.
Therefore, LLIF has the advantage that the operator can adjust the SSA by selecting the cage angle. In addition, LLIF can improve the radicular symptoms through indirect decompression by increasing the MDH and FH via the insertion of a cage with a higher profile than that in TLIF.
The superiority of LLIF for spondylolisthesis reduction has been reported in several studies [5,10,15], and LLIF was also reported to be effective in the reduction of even grade II spondylolisthesis [30]. However, a previous study comparing it to TLIF reported that LLIF had no advantage in terms of spondylolisthesis reduction [15]. In our study, the Postop-spondylolisthesis rate was significantly lower in the LLIF group (3.8± 3.8%) than that in the TLIF group (7.2±6.1%); therefore, LLIF resulted in a significant correction. The difference observed between the two studies may be due to differences in ligamentotactic effects. The ligamentotactic effect is a method used for the indirect reduction of a fracture by the application of a strong distraction force that is transmitted through intact ligaments and capsule [17]. It is used in degenerative disease as well as fracture [21]. During cage insertion, the cage height acts as a distraction force. The cage height used in our study (average, 13.0 mm) was higher than that used in the previous study (average, 11.2 mm); thus, a sufficient distraction force could be created for spondylolisthesis reduction via the ligamentotactic effect (Fig. 1).

Spondylolisthesis reduction in TLIF and LLIF. In preoperative state of DS, disc bulging and bucking of posterior longitudinal ligament and ligamentum flavum cause stenosis (A). TLIF improves stenosis through direct decompression of posterior elements, but it is difficult to insert of a cage with sufficient height, which is disadvantageous in terms of the spondylolisthesis reduction (B). LLIF can maximize the ligamentotaxic effect through insertion of cage with sufficient height, which indirectly decompresses the foraminal stenosis as well as corrects the DS effectively (C). TLIF : transforaminal lumbar interbody fusion, LLIF : lateral lumbar interbody fusion, DS : degenerative spondylolisthesis.
A number of studies have reported that one-level fusion can also affect the overall LL [2,3,14,20,28], however, in our study, onelevel fusion did not seem to have a significant effect on LL even though there was a significant difference in SSA between the TLIF and LLIF groups.
Finally, in our study, the changes in the spondylolisthesis rate, MDH, FH, and SSA between Postop and last f/u were significantly smaller in the LLIF group than those in the TLIF group, a finding similar to that of a previous study, suggesting that LLIF is stable over the long term [15] (Fig. 2). The cage used in LLIF was sufficiently larger and longer to contact the epiphyseal ring at both sides than the cage used in TLIF, which may have caused the changes. The difference in cage subsidence could also be due to this reason. In our study, although there was no difference in complications between the TLIF and LLIF groups, the complications in the LLIF group included symptoms associated with the surgical approach, whereas complications in the TLIF group included mechanical failure due to screw loosening. Although the number was small, screw loosening was present only in the TLIF group, which is indirect evidence of the excellent stability of LLIF. In four patients with screw loosening, the PostVAS-back, PostVAS-leg, and PostODI were 5.5±1.3, 3.5±0.8, 26.3±3.5%, respectively, which was not good. Although a significant difference in the clinical outcome was not observed due to the small numbers, a more accurate assessment will be possible in large-scale studies with longer follow-up periods.

Cases showing the largest change of reduced spondylolisthesis from immediate postoperative to last follow-up X-ray. In TLIF case, spondylolisthesis rate was 23.6% at preoperative (A), and reduced to 7.5% at immediately postoperative (B). It was slipped to 21.2% at 23 months after surgery (C). In LLIF case, spondylolisthesis rate was 28.7% at preoperative (D), and reduced to 6.7% at immediately postoperative (E). Then, it was 10.4% at 45 months after surgery (F). TLIF : transforaminal lumbar interbody fusion, LLIF : lateral lumbar interbody fusion.
The present retrospective study has several limitations. The two types of operations were performed by different two surgeons at a single hospital. Although baseline characteristics of the patients were matched, surgeon bias could not be eliminated because the treatment choice was not randomized. We did not elucidate the difference between DLIF and OLIF, which were mixed in the LLIF group. Although significant differences were observed in the parameters for long-term mechanical stability, bias was present due to the different types of pedicle screw systems between the groups. Finally, our study was relatively small and had a short follow-up period. A larger-prospective multicenter study with a longer follow- up period is necessary to provide additional data on the optimal treatment for DS.
CONCLUSION
The number of patients with DS is increasing with the aging society and the need for fusion surgery in patients with symptomatic DS is also increasing. According to the results of our study, both TLIF and LLIF showed good clinical and radiological results in patients with symptomatic DS. However, the LLIF was significantly superior to the TLIF in spondylolisthesis reduction, MDH and FH increase, and SSA correction as a result of the taller and larger angled cage and ligamentotactic effect. In addition, the LLIF showed mechanical stability of the reduction level due to the use of a cage with a greater footprint. Therefore, LLIF should be considered a surgical option before TLIF for patients with unstable DS requiring significant reduction.
Notes
No potential conflict of interest relevant to this article was reported.
INFORMED CONSENT
Informed consent was obtained from all individual participants included in this study.
AUTHOR CONTRIBUTIONS
Conceptualization : MJK, SWP Data curation : MJK Formal analysis : MJK Methodology : SWP, YBK Project administration : SWP Visualization : MJK Writing - original draft : MJK Writing - review & editing : MJK, SWP, YBK