Clinical Outcome of Patients Over 90 Years of Age Treated for Chronic Subdural Hematoma
Article information
Abstract
Objective
Chronic subdural hematoma (CSDH) is one of the most common pathology in daily neurosurgical practice and incidence increases with age. The aim of this study was to evaluate the prognostic factors and surgical outcome of CSDH in patients aging over 90 years compared with a control group of patients aging under 90 years.
Methods
This study reviewed 25 patients with CSDH aged over 90 years of age treated in our department. This group was compared with a younger group of 25 patients aged below their eighties. At admission past medical history was recorded concerning comorbidities (hypertension, dementia, ictus cerebri, diabetes, and heart failure or attack). History of alcohol abuse, anticoagulant and antiplatelet therapy, head trauma and seizures were analyzed. Standard neurological examination and Markwalder score at admission, 48 hours after surgery and 1–6 months follow-up, radiologic data including location and CSDH maximum thickness were also evaluated.
Results
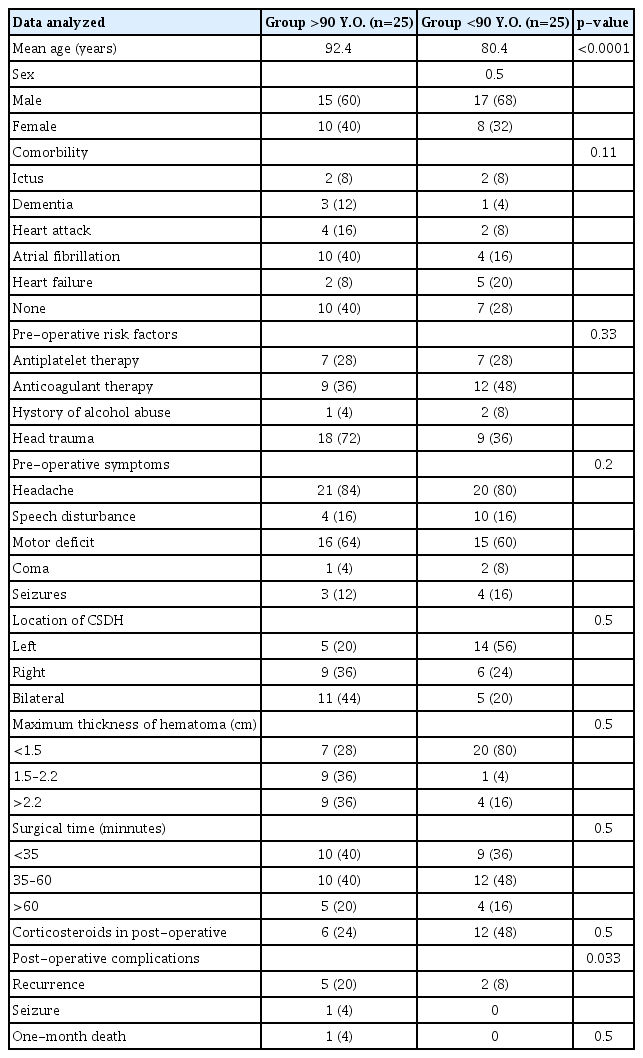
Their mean age was 92.8 years and the median was 92.4 years (range, 90–100 years). In older group, the Markwalder evaluation at one month documented the complete recovery of 24 patients out of 25 without statistical difference with the younger group. This data was confirmed at 6-month follow-up. One patient died from cardiovascular failure 20 days after surgery. The presence of comorbidities, risk factors (antiplatelet therapy, anticoagulant therapy, history of alcohol abuse, and head trauma), pre-operative symptoms, mono or bilateral CSDH, maximum thickness of hematoma, surgical time and recurrence were similar and statistically not significant in both groups.
Conclusion
In this study, we demonstrate that surgery for very old patients above 90 years of age affected by CSDH is safe and allows complete recovery. Comparing two groups of patients above and under 90 years old we found that complication rate and recovery were similar in both groups.
INTRODUCTION
Chronic subdural hematoma (CSDH) is a collection of blood in the subdural space typically found in elderly and rarely in young population. The incidence of CSDH increases with age : 3.4 per 100000 person-year in people under 60 years of age and 58–80 cases per 100000 person-year in people above 65 years of age [1,3,8,13-15,24]. Surgery is the treatment of choice for CSDH, but in patients over their nineties clinical outcome after surgical treatment is not well investigated. This study evaluates risk factors and clinical outcome of CSDH in very elderly patients treated with surgery.
MATERIALS AND METHODS
This study reviewed 25 patients with CSDH aged over 90 years of age treated in Department of Neurosurgery, Polytechnic University of Ancona, over a period of 5 years, between 2012 and 2016. This group was compared with a control group of 25 patients with an age ranging from 75 to 85 years operated for symptomatic CSDH in the same period.
Surgical indications included symptomatic CSDH with radiological signs of space-occupying intradural lesion with midline shift over 1 cm (Fig. 1). All asymptomatic patients aging over 90 years-oldaffected by CSDH were treated conservatively. The only contra-indication for surgery in symptomatic patients was the use of anticoagulant therapy or patients with Alzheimer’s disease or severe dementia.

A and B : Pre-operative and post-operative computer tomography scan images depicting bilateral CSDH in a patient aging over 90 years old. CSDH : chronic subdural hematoma.
CSDH radiological diagnosis was obtained by computer tomography (CT) scan. At admission past medical history was recorded concerning comorbidities (hypertension, dementia, ictus cerebri, diabetes, and heart failure or attack). History of alcohol abuse, anticoagulant and antiplatelet therapy, head trauma and seizures were analyzed. Standard neurological examination and Markwalder score [18] at admission was used for clinical evaluation, radiologic data including location and CSDH maximum thickness were also evaluated. Under local anesthesia, a single or double burr hole craniotomy was performed and the hematoma was evacuated by irrigation with physiological saline solution, followed by placement of a subdural closed system drain. The drain was removed 48 hours after surgery and routine CT scan was performed at 48 hours and at 30-day follow-up. Surgical time, use of steroids after surgery and post-operative complications, such as recurrence, were also evaluated.
The outcome was assessed with Markwalder score system 48 hours after surgery and at one and sixth months follow-up. The outcome was dichotomized in favorable outcome (Markwalder grade 0–1) and unfavorable outcome (Markwalder grade 2–4) (Table 1).
For comparing of characteristics of both group we used a chi-square test for comparison of non-parametric data. Comparison of quantitative parameters was performed using a ttest. Statistical tests were performed using SPSS software (IBM, Chicago, IL, USA).
RESULTS
Data about 25 super aged patients operated for chronic subdural hematoma were analyzed and described in Table 2. Their mean age was 92.8 years and the median was 92.4 years (range, 90–100). In older group, the Markwalder evaluation at one month documented the complete recovery of 24 patients out of 25 without statistical difference with the younger group. This data was confirmed at 6-month follow-up (Table 3). One patient died from cardiovascular failure 20 days after surgery. In our study the number of elderly patients operated for CSDH increases during recent years (Table 4). The presence of comorbidities, risk factors (antiplatelet therapy, anticoagulant therapy, history of alcohol abuse, and head trauma), pre-operative symptoms, mono or bilateral CSDH, maximum thickness of hematoma, surgical time, and recurrence were similar and statistically not significant in both groups, as reported in Table 5.
DISCUSSION
Chronic subdural hematoma is one of the most common pathology in daily neurosurgical practice [1,8,13,15,16,20,22-25]. In this study we evaluated the outcome and risk factors in a series of 25 patients operated for CSDH aged over 90 years of age, compared with a younger control group.
The outcome in our series was overall favorable. Super-aged patients had a good functional recovery assessed with Markwalder score at 6 months : complete in 20 patients (80%) out of 25, four patients (16%) suffered mild symptoms such as gait impairment or minor disturbance of consciousness (Markwalder grade 1) with a good quality of life. One patient died from cardiovascular failure. These data, compared with the outcome of young people, showed no statistical significance. In literature, complete neurological recovery is documented in 60–90% of operated patients [1,3,4,14,19,24] but mean age is lower than our study’s one.
There have been many reports that antiplatelet and anticoagulant therapies are risk factors for CSDH and they increase its incidence [1,7,15,20,21]; in our series 64% of patients were in treatment with anticoagulant and/or antiplatelet drugs. In patients with CSDH using antithrombotic drugs, careful decision- making is compulsory, because these therapies are more common in non-traumatized CSDH patients with cerebrovascular and/or cardiovascular co-morbidities [20]. Furthermore, antiplatelet and anticoagulant drugs may increase the probability of CSDH recurrence as well as the VII factor deficit in young patients [2,8].
Many studies, reported CSDH recurrence rate around 10– 15% [3,8,13,17,25] and elderly patients had higher rate recurrence than younger ones [2,5,6,17]. In our series the recurrence rate in the elderly group was 20%. According to literature, the higher recurrence value in our series may be due to the small superaged patient sample and age selection; this data did not show statistical significance compared to younger patients.
It is well established that a head trauma, even mild, is the most common cause of CSDH with a incidence rate of 50– 80% [3]. In the elderly group, history of mild head trauma was documented in 72% of patients, according to literature [2,15]. In our series one patient reported a moderate brain trauma with associated vertebral fracture treated with vertebral stabilization [9-11]. After one month the patient developed CSDH operated with complete recovery.
The most frequent presenting symptoms were consciousness disturbance and hemiparesis; in most cases CSDH diagnosis was delayed because neurological symptoms in superaged patients are frequently related to vascular disease or dementia. In our series the hematoma was bilateral in 44% of elderly patients; this data is not comparable with rates between 16 and 20% of other series [14] where the mean age was lower than our study’s one. The high percentage of bilateral hematoma may be related to the frequent brain atrophy of elderly people [13,24,26]. The hematoma thickness was over 2.2 cm in 36% of patients and this may be related to their brain atrophy which let large blood collection in subdural space and delays symptoms recognition [24,26].
The complication rate in the perioperative period was low. Careful pre-operative evaluation of patient’s physical status may be related to this data, meaning that the patient’s general condition represents one of the most important factors postoperative outcomes.
The overall mortality rate associated with burr-hole surgery for CSDH in literature ranges between 0.21% to 27.5%; in our study of super-aged patients, mortality rate was 4%, in line with literature [4,12,14,17,19,24,25]. Despite the small sample size of this series, these findings suggest that surgical treatment for CSDH is safe and effective even for patients ageing over 90 years-old.
CONCLUSION
In this study, we demonstrate that surgery for very old patients above 90 years of age affected by CSDH is safe and allows complete recovery; this is obtained when the patient’s physical status is fair and surgical indications and comorbidities are properly analyzed. Comparing two groups of patients above and under 90 years old we found that complication rate and recovery were similar in both groups.
Notes
No potential conflict of interest relevant to this article was reported.
INFORMED CONSENT
Informed consent was obtained from all individual participants included in this study.
AUTHOR CONTRIBUTIONS
Conceptualization : MD Data curation : AM Formal analysis : DN Methodology : MD Project administration : MS Visualization : FM Writing - original draft : VL, RB Writing - review & editing : MD, MDC