Changes in Disc Height as a Prognostic Factor in Patients Undergoing Microscopic Discectomy
Article information
Abstract
Objective
Some patients with disc herniation who underwent discectomy complain of back pain after surgery and are unsatisfied with the surgical results. This study aimed to evaluate the relationship between preoperative disc height (DH), postoperative DH, and pain score 12 months after surgery in patients who underwent microdiscectomy for herniated lumbar disc.
Methods
This study enrolled patients who underwent microdiscectomy at a medical center between January 2012 and December 2020. Patients with X-ray or computed tomography and pain score assessment (visual analog scale score) prior to surgery, immediately post-op, and at 1, 6, and 12 months after surgery were included. The DH index was defined as DH/overlying vertebral width. The DH ratio was defined as the postoperative DH/preoperative DH. Simple linear regression and multivariate linear regression analyses were applied to assess the correlation between DHs and leg pain scores 12 months after surgery.
Results
A total of 118 patients who underwent microdiscectomy were included. DH decreased up to 12 months after surgery. The DH ratio at 1, 6, and 12 months after discectomy showed a significant positive correlation with the pain scores at 12 months after discectomy (1 month : p=0.045, B=0.52; 6 months : p=0.008, B=0.78; 12 months : p=0.005, B=0.69). Multivariate linear regression analysis revealed that the level of surgery, sex, age, and body mass index had no significant relationship with back pain scores after 12 months.
Conclusion
In patients who underwent microdiscectomy, the DH ratios at 1, 6, and 12 months after surgery were prognostic factors for back pain scores at 12 months after surgery. Aggressive discectomy is recommended for lower postoperative DH ratios and Visual analog scale scores, leading to improved patient satisfaction.
INTRODUCTION
Lumbar discs play a crucial role in providing essential support for maintaining upright posture and enabling a wide range of movements. However, degenerative changes in the lumbar disc lead to functional loss, resulting in the protrusion or herniation of the nucleus [19]. A herniated lumbar disc (HLD) can compress nerve roots, leading to symptoms such as low back pain, dermatomal radiating pain, paresthesia, or neurogenic claudication. Various independent risk factors for lumbar disc herniation have been identified, including smoking, occupational lifting, and obesity [11,18,30].
Despite faster and more significant improvement in symptoms observed with surgical treatment, 17.6% of patients continue to experience pain due to recurrent HLD [21]. Recent studies have indicated that higher body mass index (BMI), history of smoking, and greater preoperative disc height (DH) are risk factors for recurrent HLD [2,4,14,23]. Additionally, 3–36% of patients experience low back pain post-discectomy, which results in poor satisfaction [20,22]. The causes of postoperative low back pain are presumed to include mechanical pain from instability, nociceptive pain resulting from a torn annulus, or incorrect patient selection; however, this has yet to be clarified [12].
Considering that lower back pain after discectomy is a significant postoperative complication Iorio-Morin et al. [12] identified six factors (female sex, low education level, marriage, not employed, low expectations of low back pain improvement, and low preoperative back pain) that predict poor outcomes for low back pain after discectomy. Another study demonstrated a relationship between reduction in DH and improvement in back pain after discectomy [7]. Notably, the number of discs removed during surgery correlates with a postoperative decrease in DH [3]. Evaluating the relationship between preoperative and postoperative DH and prognosis can provide valuable insights into the extent to which disc removal can be performed during surgery. This study aimed to assess the relationship between preoperative DH, postoperative DH, and pain scores at 12-month follow-up in patients treated with microdiscectomy for HLD.
MATERIALS AND METHODS
Since the data were extracted retrospectively and anonymized, the requirement for informed consent was waived by the Institutional Review Board (IRB) of Hanyang University Hospital (IRB file No. : HYUH 2023-05-007).
Study design
This retrospective cohort study involved a review of the medical records of patients who underwent single-level microscopic discectomy at a medical center between January 2013 and February 2021. Two neurosurgeons performed microscopic discectomies. Preoperative computed tomography (CT) and magnetic resonance imaging were conducted 2 months before surgery, and postoperative anteroposterior and lateral radiographs were obtained on the day of surgery. Follow-up visits were scheduled for patients 1, 6, and 12 months after surgery to undergo CT and X-ray evaluations. None of the patients had undergone postoperative rehabilitation.
Inclusion and exclusion criteria
All patients who underwent microscopic discectomy and attended an outpatient clinic 1 year after surgery were included in the study, regardless of age. The exclusion criteria were as follows : 1) incomplete medical records (e.g., absence of pain scores at any time point); 2) postoperative complications such as infection, postoperative hematoma, or wound dehiscence; and 3) history of spinal surgery at other levels or underlying spondylosis.
Surgical procedures
All patients underwent conventional microscopic discectomy under general anesthesia. The patients were placed in the prone position, and the corresponding laminae were exposed through periosteal dissection. A partial laminectomy was performed after the application of a retractor. The ligamentum flavum was removed, and the corresponding nerve root was confirmed. The posterior longitudinal ligament was cut at the peak of disc herniation, and the herniated mass and disc material were removed as aggressively as possible. Following removal of the herniated disc, careful confirmation was made to ensure full decompression of the affected nerve root with no residual disc around the level.
Clinical variables and radiological assessment
Clinical data such as the level of discectomy, prior surgical history, and Visual analog scale (VAS) score for back pain at each time point (before and after surgery, and at 1, 6, and 12 months after discectomy) were recorded.
Radiological variables were measured by two medical doctors specializing in neurosurgery. Measurements were primarily based on CT images, except for immediate postoperative X-rays. DH was measured as the average of the anterior, middle, and posterior DHs. The DH index (DHI) was defined as DH divided by the overlying vertebral body width. The DH ratio at each time point was calculated by dividing the DHs at each time point by the preoperative DH (Fig. 1).
Statistical analysis
Baseline patient data are presented as mean±standard deviation (range of variables), medians (%), or numbers (%). We conducted a simple linear regression test to determine which variables (standardized DH and DH ratio at each time point) showed a relationship with the pain scores at 12 months. Furthermore, to adjust for other variables, multivariate linear regression analysis was performed between the pain score at 12 months after surgery and variables with significant relationships in the linear regression test. All analyses were performed using SPSS ver. 24.0 (released 2016, IBM SPSS Statistics for Windows; IBM Corp., Armonk, NY, USA) and R version 4.1.2 (R Foundation for Statistical Computing, Vienna, Austria; http://cran.r-project.org/).
RESULTS
In total, 153 patients who underwent microdiscectomy for HLD were included in the database. Among them, 35 patients were excluded for the following reasons : 19 for missing VAS scores in medical records, three for postoperative infection, one for postoperative hematoma, six for having a previous lumbar surgery history, and six for spondylosis at other levels. Ultimately, 118 patients were included in the final analysis. Patients who missed outpatient follow-ups at each time point were also excluded.
The average age of the patients was 51.03±14.50 years, and the cohort comprised 59 male and 59 female patients before surgery. The most common disc herniation site was L4-L5, occurring in 60 patients (50.8%), followed by L5-S1 in 44 patients (37.3%). The average BMI before surgery was 23.90±3.45 (Table 1).
The mean DH measured on postoperative radiographs was 11.77±2.56 mm, which was slightly higher than the 10.32±2.03 mm measured preoperatively, possibly because the DH was measured using X-ray images immediately after surgery, at which point the DHI was slightly reduced (from 0.31 mm to 0.30 mm). In follow-up radiographs, height tended to decline over time, from 9.45±1.81 mm at 1 month after surgery to 7.41±3.75 mm at 12 months after surgery.
The DHI showed a similar tendency to decrease as the DH. The DHI was the highest preoperatively at 0.31±0.06 and gradually decreased to 0.22±0.10 at 12 months after surgery (Table 1).
The patients experienced the most severe pain before surgery, with an average VAS score of 7.59±0.72. Although the average VAS score at 12 months after surgery decreased to 2.96 ±1.77, three patients showed no improvement in the degree of preoperative pain even 12 months after surgery. Furthermore, 20 patients complained of back pain, which worsened 1 month after surgery (Table 1).
Simple linear regression analysis demonstrated that patients with larger DH ratios at 1 (B=0.52, p=0.045), 6 (B =0.78, p=0.008), and 12 months (B=0.69, p=0.005) experienced more severe pain at 12 months after surgery. However, the DH ratio immediately after surgery showed no significant effect on the pain scores at 12 months. Moreover, DHI showed no significant effect in predicting the pain score at 12 months (Table 2).
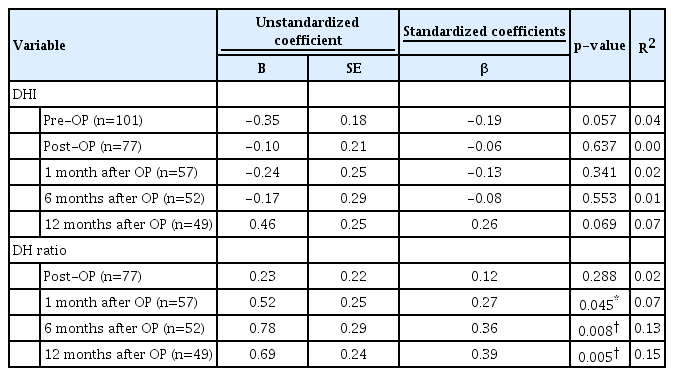
Simple linear regression analysis of the DHI or DH ratio at each time point with pain scores at 12 months after surgery
Multivariable linear regression analysis was performed using each variable that was significantly related to the pain score at 12 months. The level of surgery, sex, age, and BMI were included as covariates in the analysis. As shown in Table 3, other covariates at each time point showed no significant relationship with the pain scores at 12 months. We also found that patients with a higher DH ratio 1 month after surgery experienced more severe pain 12 months after surgery (B=0.60, p=0.027). The DH ratios at 6 and 12 months after surgery showed a similar relationship to that at 1 month (6 months : B=0.83, p=0.017; 12 months : B=0.77, p=0.003) (Table 3 and Fig. 2).

Simple linear regression analysis of the data in Table 1 demonstrates the effects of ratio of disc height (DH) at each time point on pain scores at 12 months after surgery. A : DH ratio immediately after surgery has no significant effect on pain scores at the 12-month follow-up. DH ratios at (B) 1 month, (C) 6 months, and (D) 12 months after surgery showed a positive correlation with pain scores at 12 months after surgery.
DISCUSSION
As the number of patients undergoing discectomy increases, numerous studies have been conducted to identify factors related to postoperative pain. Silverplats et al. [22] reported that a quick return to daily life results in better outcomes for back pain. Iorio-Morin et al. [12] also identified the following six clinical factors associated with poor back pain improvement after surgery : low expectations, not working, low level of education, female sex, and being married. Additionally, Tabibkhooei et al. [26] reported that higher BMI and neurological claudication are predictive factors for poor reduction in back pain. In the present study, we found that a greater reduction in DH after surgery was associated with greater improvement in postoperative back pain. Specifically, changes in DH at 1 and 6 months after discectomy were significantly associated with back pain scores at 12 months after surgery.
Brinckmann and Grootenboer [3] previously reported that DH decreases by approximately 0.8 mm per gram of removed disc tissue after disc resection. A lower DH ratio after surgery indicated that more nuclei had been removed. Therefore, we interpreted that the lower the DH after surgery, the more aggressive the disc removal. However, the optimal amount of herniated disc that should be removed to achieve better outcomes remains unclear. In two studies, McGirt et al. [15,16] compared the outcomes of two groups : aggressive discectomy and limited discectomy. In a meta-analysis, the incidence of recurrent disc herniation after limited discectomy (mean, 7%) was twice as high as that after aggressive discectomy (mean, 3.5%) [15]. In contrast to the low rate of recurrence of disc herniation, patients with a higher volume of removed disc showed a higher recurrence of back or leg pain (mean, 27.8%) than patients with a lower volume removed (mean, 11.6%) in the long-term (>2 years) follow-up. Conversely, Carragee et al. [6] stated that back pain scores in the aggressive discectomy group were worse than those in the limited discectomy group. Carragee et al. [6] compared 30 patients treated with aggressive resection to 46 patients treated with limited discectomy. Although the reherniation rate was lower in the aggressive discectomy group (9% vs. 18%), back pain scores were higher in the aggressive discectomy group at the 12-month follow-up (p=0.02). However, all surgeries in the Carragee et al.’s study [6] were performed by a single surgeon (E.J.C.), and limited discectomy was performed before 1999, whereas aggressive discectomy was performed between 1999 and 2001. Furthermore, since the age of the patients was less than 65 years, it was considered that degenerative changes and adhesions in the subtotal discectomy group had a greater effect on pain.
There is much debate in literature about whether aggressive or limited discectomy is preferable. Some studies suggest that decrease in DH associated with aggressive discectomy may cause segmental instability and thus accelerate spondylosis [25,29]. In order to reduce the segmental instability and minimize damage to surrounding normal structures, limited discectomy which removes only extruded fragments can be performed [24,28]. Many studies have argued that there is no significant difference in complications, surgical outcomes and recurrence rates between limited discectomy and aggressive discectomy, while also highlighting shorter operating time and reduced short-term postoperative back pain [1,9,25,27]. Therefore,there is a growing trend towards favoring limited discectomy in recent times. However, in cases where there is a high risk of reherniation, such as when the size of annular defect is large, aggressive discectomy may be necessary rather than fragmentectomy [5,8,13,17]. In cases where nucleotomy is needed, we believe that, removing more disc materials which results in a lower DH after surgery, may lead to better clinical outcomes.
As DH decreases after surgery, the height of the intervertebral foramen and movement between the vertebrae also decrease. Decreases in relative movement result in alleviation of motion-related back pain in the early stages after surgery. Thus, the greater the DH reduction, the smaller the micromovement, and the greater the improvement in pain scores. However, as DH decreases over time, micro-movement and facet loading may lead to adhesions and hyperplasia of the joints [7,10]. This causes patients to complain of back pain, even during long-term follow-up. This is consistent with the significant decrease in pain scores one month after surgery observed in the current study. Additionally, this would explain the similarity in pain scores at 6 and 12 months after surgery in this study. Back pain after approximately 6 months is considered to originate from adhesion and hyperplasia of the joints and does not show much improvement over time.
There are several methods to estimate DHI, such as the ratio of DH/overlying vertebral height, the ratio of DH/overlying vertebral width, and the average of the anterior and posterior DH. In the present study, the DH/overlying vertebral width ratio was used to standardize the DHs, which varied from patient to patient. The DH/overlying vertebral height ratio was not used because the height could be variable for other reasons, such as compression fractures.
This retrospective study aimed to gain a greater understanding of the causes of postoperative back pain and establish the degree of discectomy. However, this study has some limitations. First, only pain scores for lower back pain were considered, and information related to radiating pain was excluded. Since most radiating pain after discectomy is explained by sequelae of compressed nerve roots or reherniation of the intervertebral disc, it shows little relationship with DH. To ensure a clear analysis, it is necessary to assess the relationship between DH and radiating pain. This study also did not take into account underlying medical conditions, socio-economic factors such as occupation, alcohol use, smoking status, or psychological factors. Second, although surgeries were performed according to the established protocol, there could be differences in nuclear manipulation depending on the surgeon. Furthermore, the effect of the surgeon’s manipulation method was not considered in the present study. Thirdly, since all surgeries in this study were aggressive discectomy, it is challenging to compare the outcomes of this study and that of sequestrectomy directly. Finally, the single-center retrospective design of this study could have introduced inevitable bias. Nevertheless, the sample size of this study was relatively large compared with that of studies with similar patients. In a meta-analysis by Chen et al. [7], the average number of patients in the 19 included studies was approximately 45. Further multicenter studies are required to confirm the relationship between DH and back pain after discectomy.
CONCLUSION
The present study demonstrated that changes in DH are a prognostic factor for pain in patients undergoing microscopic discectomy. Patients who experienced a greater reduction in DH after surgery showed better improvement in back pain scores 12 months postoperatively. Careful consideration of the changes in DH and their potential effects on long-term back pain is warranted in patients undergoing microscopic discectomy. However, further studies are needed to identify additional factors that affect the outcomes of microscopic discectomy and optimize surgical techniques for better patient outcomes.
Notes
Conflicts of interest
No potential conflicts of interest relevant to this study exist.
Informed consent
This type of study does not require informed consent.
Author contributions
Conceptualization : MK, HJC, KHB; Data curation : MK, HJC, KSC, KHB; Formal analysis : MK, HJC, HJY, MHH; Methodology : MK, HJC, MHH, MKN; Project administration : MK, HJC; Visualization : MK, HJC, MKN; Writing - original draft : MK, HJC, KSC; Writing - review & editing : MK, HJC, HJY
Data sharing
None
Preprint
None



