Biomechanical Comparison of Spinal Fusion Methods Using Interspinous Process Compressor and Pedicle Screw Fixation System Based on Finite Element Method
Article information
Abstract
Objective
To investigate the biomechanical effects of a newly proposed Interspinous Process Compressor (IPC) and compare with pedicle screw fixation at surgical and adjacent levels of lumbar spine.
Methods
A three dimensional finite element model of intact lumbar spine was constructed and two spinal fusion models using pedicle screw fixation system and a new type of interspinous devices, IPC, were developed. The biomechanical effects such as range of motion (ROM) and facet contact force were analyzed at surgical level (L3/4) and adjacent levels (L2/3, L4/5). In addition, the stress in adjacent intervertebral discs (D2, D4) was investigated.
Results
The entire results show biomechanical parameters such as ROM, facet contact force, and stress in adjacent intervertebral discs were similar between PLIF and IPC models in all motions based on the assumption that the implants were perfectly fused with the spine.
Conclusion
The newly proposed fusion device, IPC, had similar fusion effect at surgical level, and biomechanical effects at adjacent levels were also similar with those of pedicle screw fixation system. However, for clinical applications, real fusion effect between spinous process and hooks, duration of fusion, and influence on spinous process need to be investigated through clinical study.
INTRODUCTION
The lumbar arthrodesis is a prevalent surgical treatment for degenerative disc disease. Lumbar arthrodesis has many advantages such as high fusion rate, preservation of the original disc height, and maintained stability of lumbar spine2). The pedicle screw fixation system implemented by posterior lumbar interbody fusion (PLIF) method has been widely used and regarded as gold standard for lumbar arthrodesis9). Although pedicle screw fixation system is a popular surgical treatment for degenerative disc disease, high complication rates have been reported. It is reported that the surgical procedure to implement the pedicle screw fixation system is technically demanding and many complications have been observed11). The most frequently detected complications are screw misplacement and pedicle breakage during surgical operation. Also, postoperative complications include screw loosening, breakage, and loss of correction. Besides complications related to screw insertion, large blood loss and wound infection have also been identified48). For these reasons, the use of pedicle screw fixation system may need to be limited by considering patient's age and bone condition.
In order to minimize such complications, interspinous spacers such as X-stop and Coflex have been developed without using screw insertion131823). The Coflex system has been widely investigated through finite element analysis and clinical studies. As a dynamic stabilization system, Coflex preserves the motion range compared to pedicle screw fixation system and is less invasively inserted with convenient surgical process17). The complications including fracture of spinous process or implant after inserting Coflex were also investigated in previous studies37). Recently, one of interspinous devices, Interspinous Process Compressor (IPC), has been introduced, approved by Korean Food and Drug Administration (KFDA), and commercially released as TieGER™ (ANT technology, Yongin, South Korea). The IPC has a unique geometry that is different from other interspinous process spacers as shown in Fig. 1. It consists of a bone block that is inserted between spinous processes and hooks that are fixed on each spinous process, in order to completely fuse the lumbar segments. Although this new spinal fusion implant is expected to have advantages such as reduced damages to ligaments, muscles and vertebrae as the implant is laterally inserted less invasively and screws are not used to fix with vertebrae, the biomechanical effects after the fusion of lumbar segments with the IPC have not been investigated.
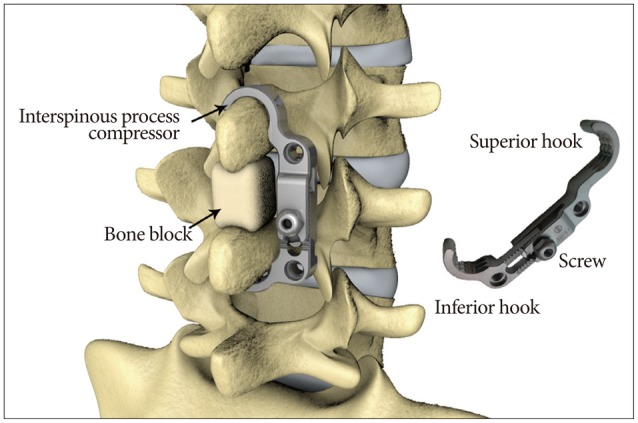
Geometry of the proposed interspinous process compressor device, which consists of bone block, superior hook, screw, and inferior hook.
The purpose of this study is to investigate the biomechanical effects of the proposed IPC system using finite element analysis before clinical studies. The biomechanical effects such as range of motion (ROM), intervertebral disc stress, and facet contact force of IPC system were investigated and compared with conventional pedicle screw fixation system.
MATERIALS AND METHODS
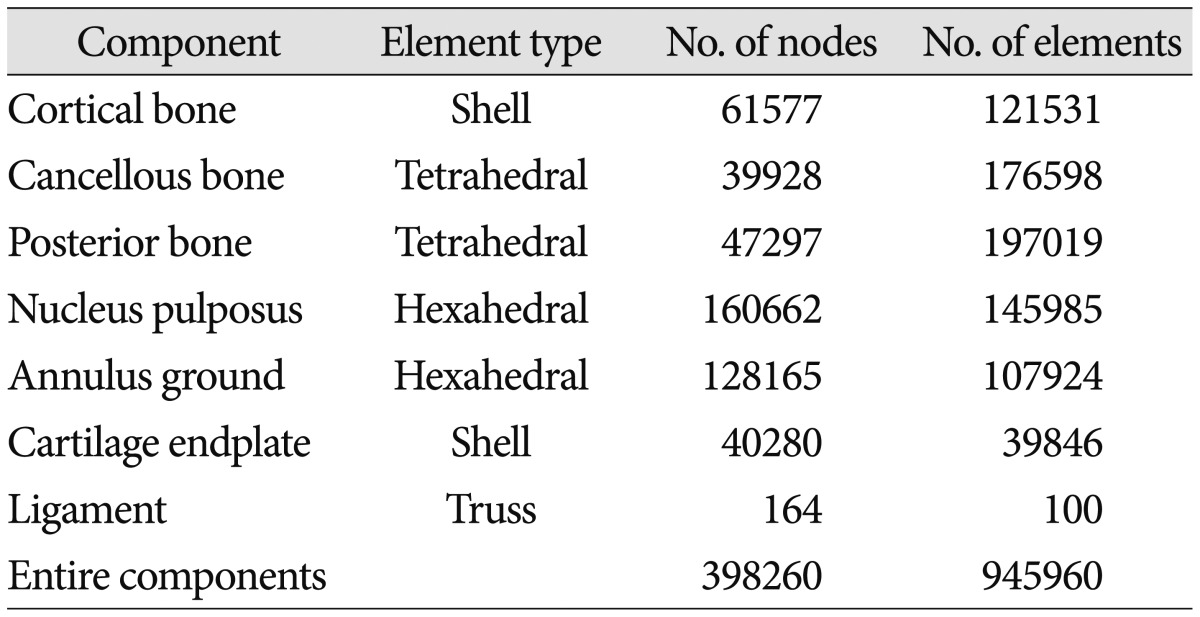
The computed tomographic scan data of a healthy 24-years-old male was taken and reconstructed to three dimensional geometry using Mimics software (Materialise Inc., Leuven, Belgium). The 3D geometry was imported to Hypermesh software (Altair Engineering Inc., Troy, MI, USA) and converted from surface to solid type. Then, it was meshed with finite elements. The element types, number of nodes and elements of each component are shown in Table 1. The cortical bone was constructed from the surface of cancellous bone with a thickness of 1 mm and cartilage endplate was extracted from the surface of intervertebral disc with a thickness of 0.5 mm. The final finite element (FE) model had five vertebras (L1–5), four intervertebral discs, cartilage endplates, and ligaments. The total number of nodes and elements were 398260 and 945960, respectively.
The material properties of each component were obtained from the literature, as shown in Table 2. Nucleus pulposus has nearly incompressible property. Annulus fibrous ground was modeled to be linear elastic. Ligaments were modeled to be linear elastic and they can resist tension only. The FE model was exported to Abaqus software (ABAQUS 6.13; Hibbitt, Karlsson & Sorenson, Inc., Providence, RI, USA) after the material properties were applied to each component of lumbar spine in the model. The frictionless sliding contact condition was applied to the surface of facet joints. The developed 3-dimensional FE model as shown in Fig. 2A was validated by comparing ROM at each intervertebral segment in extension, flexion, lateral bending and axial torsion based on the study by Yamamoto et al.28).
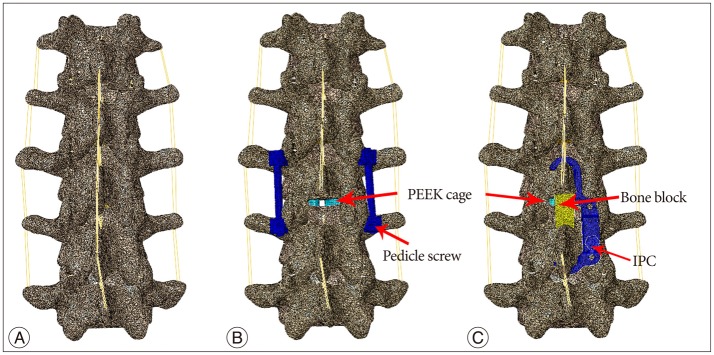
Finite element models of lumbar spine with no implant (A), PEEK cage and pedicle screw implemented by posterior lumbar interbody fusion method (B) and PEEK cage and interspinous process compressor systems (C). PEEK : polyether ether ketone.
In order to compare the biomechanical changes after spine fusion, two types of surgical models, PLIF and IPC models, were developed based on the validated intact spine model. The PLIF model consisted of polyether ether ketone (PEEK) cages, pedicle screws, and rods as shown in Fig. 2B. The length and diameter of the pedicle screw were 45 mm and 6 mm, respectively. The geometry of pedicle screws was approximated as cylinder in order to simplify the simulations. Following the standard surgical method, supraspinous ligament, interspinous ligament, and posterior longitudinal ligament at surgical level were removed, and inferior portion of L3 lamina was also removed. The PEEK cage was inserted between L3 and L4 after intervertebral disc was totally resected. After the cage was inserted, the pedicle screw fixation system was implanted at L3–4 level. The tie interaction was applied to cage and vertebral bodies for the complete fusion. Also, pedicle screws were entirely tied to the vertebral bodies.
Next, the IPC model consisted of PEEK cage, bone block, inferior hook, superior hook, and screw that combines superior hook with inferior hook, as shown in Fig. 2C. The size of bone block and length of the hooks were adjusted to fit the developed FE model. The surgical procedure was the same as with the PLIF model. The PEEK cages were inserted at the same place as with the PLIF model. The bone block was inserted between spinous process of L3 and L4. The superior and inferior hooks were placed on spinous processes of L3 and L4. The hooks were connected with screw and tied so that hooks cannot be separated. The tie interaction was applied to all spinal implants and vertebral bodies for the complete fusion condition.
Two loading conditions were used in this study. The first loading condition was for validation of the intact FE model, following the same protocol used in the study of Yamamoto et al.28). The pure moment of 10 Nm was applied to the superior surface of L1 while the inferior surface of L5 was fixed in all directions. The second loading condition was applied to both intact and surgical models to analyze the biomechanical changes caused by the surgical implants. The follower load of 280 N that represents partial body weight along the curvature of lumbar spine was applied21). The truss elements were attached bilaterally along the curvature of lumbar spine as previous studies1215). For surgical models, adjusted moments were applied to superior surface of L1 to obtain same lordosis (L1–5) that was calculated with the intact model where the moment of 10 Nm was applied. The moment that causes the same lordosis with intact spine was investigated in each loading condition5). The identified moments to apply to both surgical models under extension, flexion, bending, and torsion were 16 Nm, 12.6 Nm, 11 Nm, and 13.5 Nm, respectively. The validation of intact FE model and biomechanical changes caused by the surgical implants were investigated in flexion, extension, lateral bending and axial torsion conditions.
RESULTS
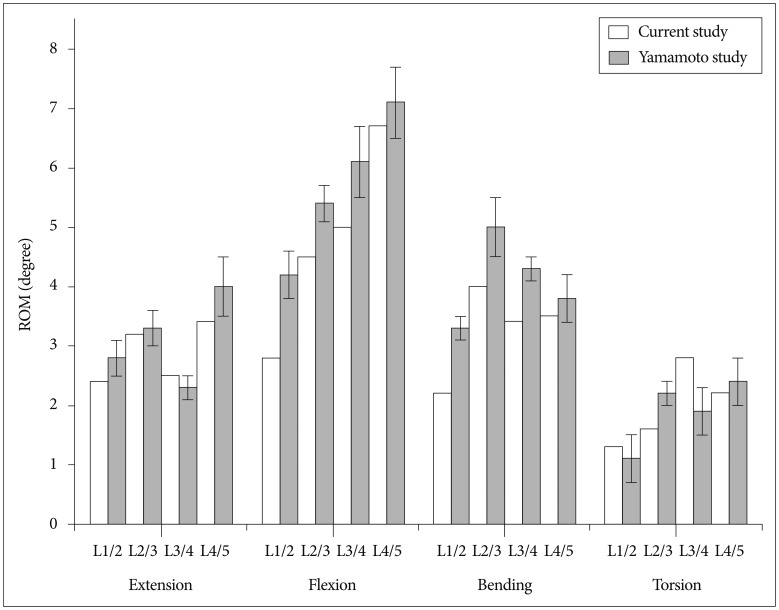
To validate the constructed intact spine model, the ROM of finite element model of intact spine was compared with the results of the study by Yamamoto et al.28) The results were within ±1 degree of the ROM values reported in Yamamoto et al.'s study in extension, flexion, bending, and torsion, as shown in Fig. 3.
In Fig. 4, the ROM at adjacent levels (L2/3, L4/5) and surgical level (L3/4) was compared among intact and surgical models in extension, flexion, lateral bending, and axial torsion. The ROM of both surgical models remarkably decreased at surgical level (L3/4) compared to the intact model in all motions. The ROM at surgical level was changed by -96% and -94% in extension, -96% and -95% in flexion, -92% and -89% in bending, and -87% and -88% in torsion in PLIF and IPC models, respectively, compared to the intact model. The PLIF and IPC models resulted in similar ROM at surgical level, with a difference of less than 0.1 degree. On the other hand, the ROM increased in all motions at adjacent levels (L2/3, L4/5). The ROM at L2–3 level was changed by +10% and +14% in extension, +29% and +30% in flexion, +6% and +8% in bending, and +61% and +61% in torsion in PLIF and IPC models, respectively, compared to the intact model. The ROM at L4–5 level was changed by +90% and +85% in extension, +30% and +30% in flexion, +9% and +9% in bending, and +54% and +50% in torsion in PLIF and IPC models, respectively, compared to the intact model. The ROM was more increased at L4/5 level than L2/3 level in both surgical models and the surgical models had similar ROM, with a difference within 0.1 degree at adjacent levels.
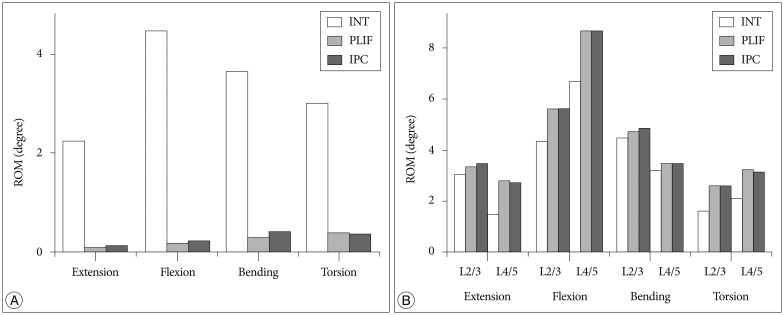
ROM of the PLIF and IPC models at surgical level (L3/4) (A) and adjacent levels (L2/3, L4/5) (B) in extension, flexion, bending and torsion, compared to the intact model. ROM : range of motion, INT : intact transverse ligament, PLIF : posterior lumbar interbody fusion, IPC : Interspinous Process Compressor.
The stress in intervertebral discs was compared in Fig. 5, among intact and surgical models at adjacent levels (L2/3, L4/5), which are represented as D2 and D4. The stress in D2 was changed by -3% and +3% in extension, +20% and +20% in flexion, -0.4% and +3% in bending, and +12% and +10% in torsion in PLIF and IPC models compared to the intact model, respectively. The stress in D2 increased with the PLIF model in flexion and torsion while it increased in all motions with the IPC model. The stress in D4 was changed by +13% and +11% in extension, +12% and +12% in flexion, +4% and +4% in bending, and -22.1% and -22.5% in torsion in PLIF and IPC models, respectively, compared to the intact model. The stress in D4 increased in both surgical models except torsion condition, compared to the intact model. The difference in intervertebral disc stress of IPC and PLIF models was 5.8% in D2 and 1.8% in D4.
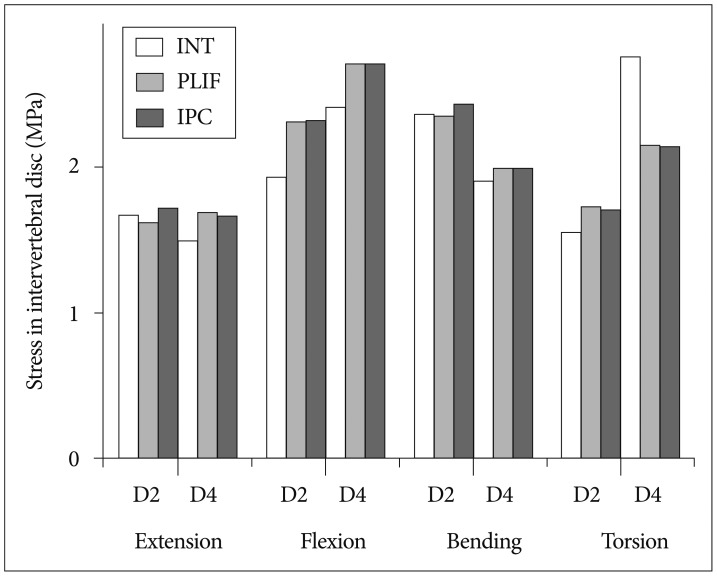
Von Mises stress in the intervertebral disc of the PLIF and IPC models at adjacent levels (D2, D4) in extension, flexion, bending and torsion, compared to the intact model. INT : intact transverse ligament, PLIF : posterior lumbar interbody fusion, IPC : Interspinous Process Compressor.
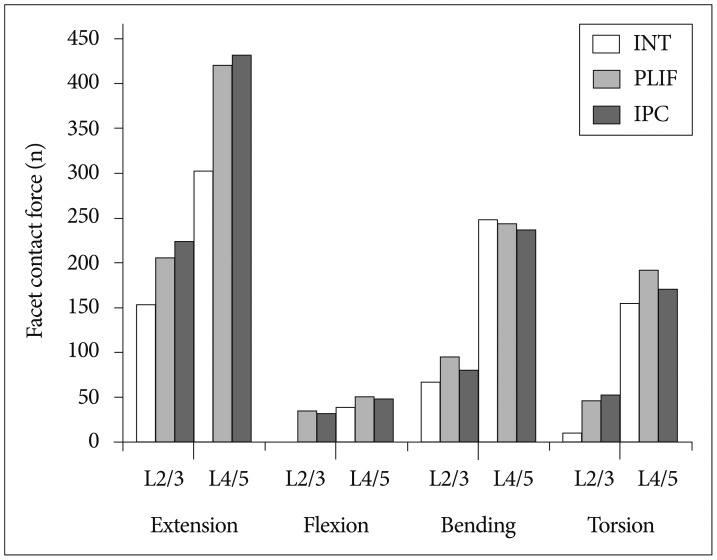
The facet contact force at adjacent levels (L2/3, L4/5) was compared in Fig. 6, among intact and surgical models. The facet contact force at surgical level was zero in all motions while it tended to increase at adjacent levels (L2/3, L4/5) in all motions for both PLIF and IPC models. The facet contact force at L2/3 level was changed by +34% and +46% in extension, +42% and +20% in bending, and +364% and +432% in torsion, in PLIF and IPC models, respectively. In flexion, the facet contact force was zero in intact model while it increased in both surgical models. The facet contact force at L4/5 level was changed by +39% and +43% in extension, +29% and +24% in flexion, -2% and -4% in bending, and +24% and +11% in torsion, in PLIF and IPC models, respectively. The maximum difference in facet contact force of PLIF and IPC models was 15.4% in bending condition.
DISCUSSION
In this study, the biomechanical changes after inserting the IPC were investigated and compared with pedicle screw fixation system using finite element analysis. We used CT images of a healthy, young male to reconstruct three dimensional geometry of lumbar spine. The characteristic of FE model of lumbar spine was represented by applying material properties of each component, based on the previous FE studies as shown in Table 2. A number of previous studies also used CT images of young patient and normal condition of lumbar spine to construct the FE models3141527). In our FE model, only one level of intervertebral disc (L3/4) was assumed to be degenerative condition, and more importantly, the whole degenerative portion of intervertebral disc was removed following the standard surgical procedure as in previous studies121415). Therefore, the used FE model could be concluded to be appropriate to represent surgical model of degenerative disc disease.
As a spinal fusion device, the IPC model showed comparable biomechanical effects with the conventional PLIF model. At surgical level (L3/4), the intersegmental rotation was remarkably decreased. Accordingly, no facet contact force occurred in both surgical models. The results predicted by FEA in the current study were similar to the previous results525). The ROM values were similar between the IPC and PLIF models with a maximum difference of 0.1 degree and no facet contact force occurred in all motions for both surgical models. At adjacent level, on the other hand, the ROM and facet contact force increased according to fusion effect. These adjacent effects had been previously reported and considered as major complications of spinal fusion121415). We obtained similar results using the IPC model. The ROM was maximally changed in extension at L4/5 level in both surgical models. The ROM values were similar between the IPC and PLIF models. The facet contact force of the IPC model was slightly higher than that of the PLIF model in extension, while that of the PLIF model was slightly higher than the IPC model in other motions. In addition, stress in intervertebral discs slightly increased after spinal fusion at L2/3 or L4/5 level as previous study5). The stress in adjacent intervertebral discs of the IPC model was slightly higher than that of the PLIF model with the difference of 5.8%.
In summary, the FEA results show that the adjacent effects of using the IPC model were similar to those of using conventional pedicle screw fixation system, based on the assumption that the implants were perfectly fused with the bones. The anterior bone was fused with PEEK cage and posterior bone was also fixed with screws for PLIF model, and with bone block and interspinous compressor for IPC model. Accordingly, biomechanical effects of using PLIF and IPC methods were not essentially different in all motions.
As limitations of the current study, the spinous process and hooks were modeled to be fused as one body although the hooks were fixed with spinous process using keel in reality. Accordingly, the stress on spinous process was not analyzed, which however should be investigated in future clinical studies as complications such as fracture of spinous process can occur. The actual fusion effect between spinous process and hooks, duration of fusion, and influence on spinous process need to be investigated through clinical study. In addition, interspinous devices such as Coflex and DIAM were analyzed using finite element method in previous studies13). In those studies, the posterior parts were fused with interspinous device and the intervertebral disc was preserved. On the other hand, in our study, the intervertebral disc was entirely removed and PEEK cages were inserted instead. As a result, the biomechanical effects of the IPC system could not be directly compared to other types of interspinous devices reported in previous studies. Such comparative investigations, however, would need to be performed as future works.
CONCLUSION
A new type of spinal fusion device, IPC, was analyzed biomechanically through FEM. Based on the simulated results, it exhibited similar fusion effect at surgical level and similar biomechanical effects at adjacent levels compared to pedicle screw fixation system. The IPC with less invasive local incision and without screw insertion, resulting in reduced damages to ligaments, muscles, and vertebrae of the patient and eliminated complications associated with screws, may extensively be used regardless of patient's age and bone conditions after clinical validations for fusion rates and long term stability.
Acknowledgements
This work was presented at the 54th Annual Meeting of the Korean Neurosurgical Society on Oct. 17-19, 2014.
This research was supported by grants from the Basic Science Research Program of the National Research Foundation (NRF-2014R1A1A3050285), the Industrial R&D program of MOTIE/KEIT (10052732), and the institute of Medical System Engineering (iMSE) and the Integrative Aging Research Center of Gwangju Institute of Science and Technology (GIST), Korea.