INTRODUCTION
Central nervous system (CNS) aspergillus abscess is very rare in immunocompetent patients and a potentially life threatening disease that is usually misdiagnosed because its presentation is similar to that of a tumor. Despite advances in diagnosis and treatment in recent years, CNS aspergillus abscesses still leads to significant morbidity and mortality2,15). Early diagnosis is important for successful treatment.
A case of parasellar aspergillus extending from the cavernous sinus, which was clinically indistinguishable from the intracranial neoplasms, is presented in this report.
CASE REPORT
A 73-year-old male was admitted to our hospital with the complaints of headache persisting for approximately three months, and presented with progressive visual deterioration and ptosis in the right eye. He had no known disease and no apparent immune deficiencies. On physical examination, he was afebrile, but he had experienced unintentional weight loss and fatigue. His general condition was poor as a result of malnutrition. The neurological examination revealed a ptosis, ophthalmoplegia, and impairment of visual acuity on the right eye. His laboratory results were as follows : white cell count, 9.100/µL; sedimentation rate, C-reactive protein, peripheral smear and biochemical tests were all in normal range. Viral markers were negative.
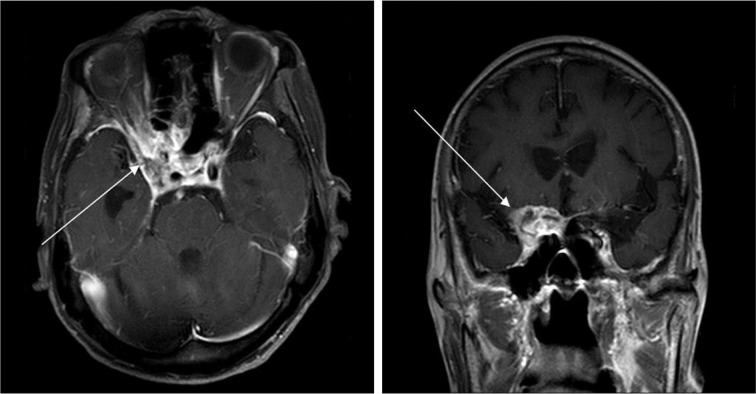
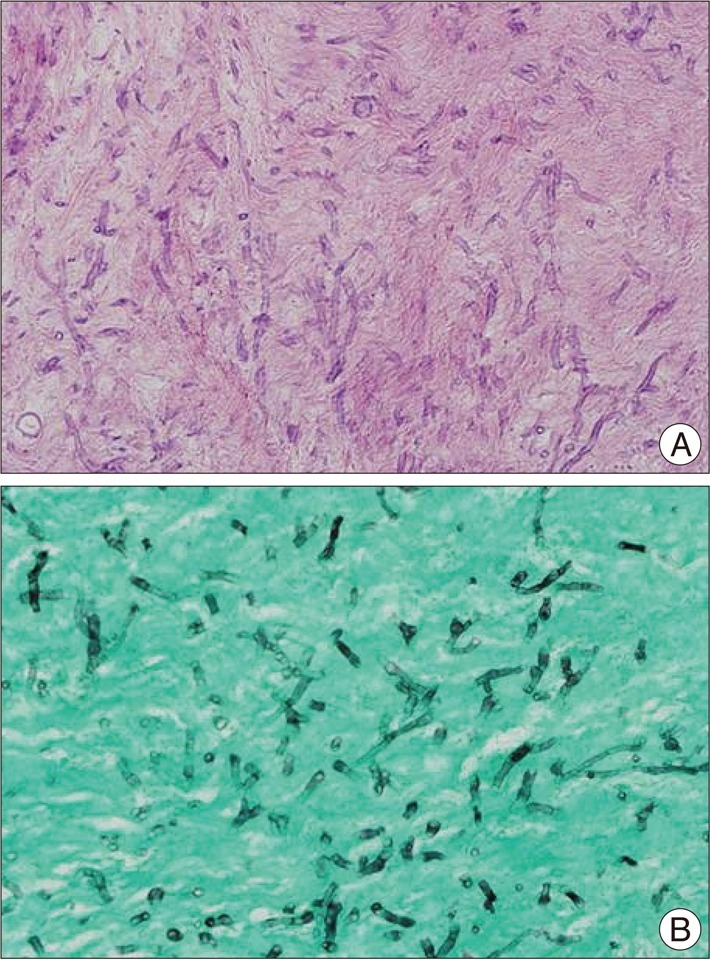
Magnetic resonance imaging (MRI) revealed a mass in the right cavernous sinus, extended to the anterior crainial fossa and the superior orbital fissure with an iso-signal intensity in T1-weighted iamge. The lesion showed a slightly low signal intensity in T2-weighted sequences and strong enhancement (Fig. 1). Based on these MRI findings, the impression was inflammatory abscess, but meningioma or metastatic tumor were also suspected. The patient underwent a pterional approach craniotomy for pathologic diagnosis and decompression of neural structures. During surgery, a well-encapsulated pus pocket was found at the clinoid process, and severe adhesion with the surrounding tissue was encountered. An intra-operative frozen biopsy revealed a fungal infection. The biopsy material showed inflammatory granulation tissue and micro abscesses containing a large number of hyphae with 45 degree angulations and spores (Fig. 2). The pathology result was consistent with aspergillus infection.
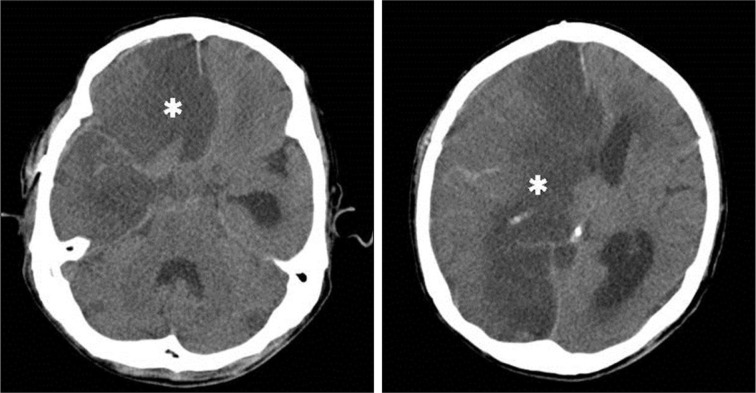
Postoperatively, the patient was treated by systemic administration of antifungal drug (Amphotericin-B and Voriconazole), to which he showed only a minimal response. Despite appropriate medical and surgical treatment, the disease progressed and the patient eventually died from fatal cerebral ischemic change and severe brain swelling on the 23rd postoperative day (Fig. 3).
DISCUSSION
CNS aspergillosis is rare. However, the number of reported cases increased significantly in the last decade (Table 1)7,10-14,16,19). Aspergillus can reach the CNS by three different routes. The first is by hematogenous spread from a remote extracranial focus. The second is by extension from a contiguous extracranial location, and the third is direct introduction of aspergillus by a neurosurgical procedure iatrogenically3).
CNS aspergillosis is very serious, with a mortality of more than 90%2,15). CNS aspergillos presents as meningitis, encephalitis, brain abscesses, subdural abscesses, mycotic arteritis or sellar abscess5).
Preoperative diagnosis of parasellar aspergillus abscess is difficult because clinical presentation and imaging findings in these patients are very similar to the symptoms and imaging results in patients with neoplasms9,17). Headaches and unilateral ophthalmologic signs, including orbital pain, visual deterioration and progressive ophthalmoplegia dominate the clinical presentation of parasellar aspergillus abscess. Ptosis is reported in up to 46% of published reports4). MRI is the best technique for the radiological evaluation of a sellar abscess, but the definitive diagnosis is made with histological tests1,8). On an MRI, the sellar abscess usually appears as a hypo-isointense sellar mass on T1-weighted sequences, as a hyperintense mass on T2-weighted sequences, and as a cystic lesion with peripheral ring enhancement after the administration of a contrast medium. In our patients, imaging findings suggested parasellar tumor, but the contrast enhanced rims of the masses and the clinical findings led us to reconsider the preoperative diagnoses.
Patients with aspergillosis have historically been treated with amphotericine B or combined therapy with amphotericine B and flucytosine or itraconazole. The superiority of voriconazole and caspofungin over amphotericin B as initial therapy for aspergillosis infection in terms of response rate, survival rate, and safety has now been demonstrated in a large randomised study6,18). The aim of treatment should be the complete removal of the masses as early as possible. Even with the invasive type, providing intra dural extension had not yet occurred, total excision was curative without systemic use of antifungal agents. However, in patients in whom total removal cannot be achieved or intra dural invasion has already been confirmed, intensive systemic therapy with antifungal agents must be administered postoperatively to prevent subsequent lethal vasculitis or meningoencephalitis developing. In our case, treatment by voriconazole and amphotericine B was effective in patient, but patient died of cerebral ischemic change, possibly due to resistance for antifungal agents, or developing vessel invasion.
CONCLUSION
Aspergillus infection is strongly invasive into vessels. It is important to consider the possible occurrence of cerebrovascular disease when treating invasion of aspergillosis into the CNS. CNS aspergillosis is very serious, with a high mortality. A combination of surgical resection and antifungal therapy resulted in good outcomes. The prognosis of the patients depends on early diagnosis and prompt aggressive treatment.