Intrawound Vancomycin Powder Application for Preventing Surgical Site Infection Following Cranioplasty
Article information
Abstract
Objective
Surgical site infection is the most detrimental complication following cranioplasty. In other surgical fields, intrawound vancomycin powder application has been introduced to prevent surgical site infection and is widely used based on results in multiple studies. This study evaluated the effect of intrawound vancomycin powder in cranioplasty compared with the conventional method without topical antibiotics.
Methods
This retrospective study included 580 patients with skull defects who underwent cranioplasty between August 1, 1998 and December 31, 2021. The conventional method was used in 475 (81.9%; conventional group) and vancomycin powder (1 g) was applied on the dura mater and bone flap in 105 patients (18.1%; vancomycin powder group). Surgical site infection was defined as infection of the incision, organ, or space that occurred after cranioplasty. Surgical site infection within 1-year surveillance period was compared between the conventional and vancomycin powder groups with logistic regression analysis. Penalized likelihood estimation method was used in logistic regression to deal with zero events. All local and systemic adverse events associated with topical vancomycin application were also evaluated.
Results
Surgical site infection occurred in 31 patients (5.3%) and all were observed in the conventional group. The median time between cranioplasty and detection of surgical site infection was 13 days (range, 4–333). Staphylococci were the most common organisms and identified in 25 (80.6%) of 31 cases with surgical site infections. The surgical site infection rate in the vancomycin powder group (0/105, 0.0%) was significantly lower than that in the conventional group (31/475, 6.5%; crude odds ratio [OR], 0.067; 95% confidence interval [CI], 0.006–0.762; adjusted OR, 0.068; 95% CI, 0.006–0.731; p=0.026). No adverse events associated with intrawound vancomycin powder were observed during the follow-up.
Conclusion
Intrawound vancomycin powder effectively prevented surgical site infections following cranioplasty without local or systemic adverse events. Our results suggest that intrawound vancomycin powder is an effective and safe strategy for patients undergoing cranioplasty.
INTRODUCTION
Cranioplasty is a surgical procedure for repairing a skull defect resulting from a previous operation or injury in order to protect the brain, improve cerebrospinal fluid dynamics, and provide a natural form of the skull. Nevertheless, cranioplasty can have serious complications, including intracranial hemorrhage, infection, seizures, bone resorption, wound dehiscence, and delayed hydrocephalus [9,16,30]. Among these complications, surgical site infection has the most detrimental effects on the brain. Although a simple scalp infection can be controlled with antibiotics, re-operation including bone flap removal is necessary when deep wound infection involving the bone flap or empyema in the epidural or subdural space occurs. Furthermore, long-term antibiotic therapy for surgical site infection can cause various medical complications. Recent studies showed that the surgical site infection rate was 3.7–26% [14,15,19,26] indicating that surgical site infection following cranioplasty is not infrequent.
One of the ideas for decreasing surgical site infection is use of topical antibiotics to the surgical wound. The rationale of using intrawound antibiotics is to achieve a local high antibiotic concentration and a high bacterial killing rate, while minimizing systemic toxicity [5]. Given that the most common organisms associated with surgical site infections are gram-positive bacteria, intrawound vancomycin has been applied in various surgical procedures including cardiac, orthopedic, and spine operations, and showed its effects and safety [5,7,10,17,21,25,28]. Based on this background, we have been using intrawound vancomycin powder in cranioplasty. The purpose of this study was to evaluate the effect of intrawound vancomycin powder application for preventing surgical site infection following cranioplasty compared with the conventional procedure without topical antibiotics.
MATERIALS AND METHODS
This retrospective study was approved by the Institutional Review Board of Bundang Jesaeng General Hospital (DMC 2022-08-010). The requirement to obtain written informed consent to participate in this study was waived. All patients with skull defects who underwent cranioplasty in our institution between August 1, 1998 and December 31, 2021 were screened for eligibility. We excluded patients who 1) underwent craniectomy at other hospitals, 2) underwent craniectomy due to infectious conditions, or 3) were lost to regular follow-up after cranioplasty. According to inclusion and exclusion criteria, 595 patients were screened and 15 patients (three underwent craniectomy at other hospitals, two underwent craniectomy for infectious conditions, and 10 were lost to follow-up) were excluded. Finally, a total of 580 patients were included in this study.
Cranioplasty was performed by making an incision along the previous incision site. Any dura defect was repaired with dura substitutes and multiple sutures water-tightly. Autologous bone or alternative material such as polymethyl methacrylate or titanium was then used to cover the skull defect along the margin of the bone defect. A hemovac line was placed on the autologous bone or alternative materials, and the scalp flap was closed. When the skull defect was not large, a hemovac was not used according to the surgeon’s decision. First-generation cephalosporin was administered intravenously for 7 days as a prophylactic antibiotic. Other antibiotics for gram-positive organisms were used in patients showing adverse effects of cephalosporin. If other antibiotics were already being used for a concomitant infection and were effective against gram-positive bacteria, the antibiotics in use were continued. In the case of intrawound vancomycin, vancomycin powder was applied on the dura mater after dura repair. A bone flap was then placed, and the remaining vancomycin powder was applied on the bone flap (Fig. 1). Intrawound vancomycin powder was applied in 105 patients (18.1%) and the conventional method without topical antibiotics was used in 475 patients (81.9%).
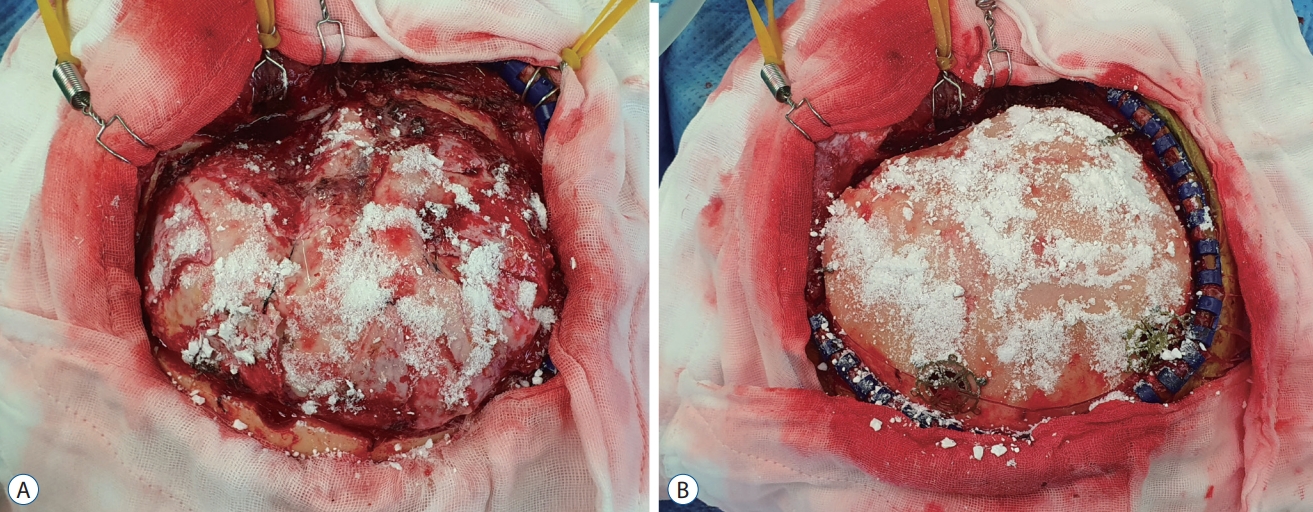
Intrawound vancomycin application. Vancomycin of 1 g is usually sufficient to cover the entire surface of the dura and bone flap. After dura defect repair, half of the vancomycin powder is applied on the dura (A). Bone flap is placed and then the remaining vancomycin powder is applied on the bone flap (B).
We collected demographic, clinical, laboratory, and procedural data of the patients. The clinical data included body mass index, medical history, history of smoking, neurological status before cranioplasty, the reason for the initial craniectomy, and post-cranioplasty antibiotics. The laboratory data included white blood cell count and C-reactive protein level before cranioplasty. The procedural data included the interval from the initial craniectomy to cranioplasty, operation time, and materials used for cranioplasty (autologous bone, polymethyl methacrylate, or titanium).
Surgical site infection was defined as infection of the incision, organ, or space that occurred after surgery, following the Centers for Disease Control and Prevention guidelines [3,20]. Craniotomy has a 90-day surveillance period for surgical site infection according to the guideline. However, because prosthetics were implanted in cranioplasty, the surveillance period in this study was extended to 1 year. As a safety parameter, all local and systemic adverse events associated with topical vancomycin application were evaluated.
The Mann-Whitney U test was used for continuous variables, and the chi-squared test or Fisher’s exact test was used for nominal variables in comparisons of baseline characteristics. Outcomes were compared between patients receiving cranioplasty using intrawound vancomycin powder and the conventional method by logistic regression analysis. The comparison was adjusted for variables showing a baseline group difference with a p-value of <0.2 and provided with an adjusted odds ratio (OR) and 95% confidence interval (CI). Penalized likelihood estimation method was used in logistic regression to deal with zero events. All statistical analyses were conducted using SAS Studio (version 3.8; SAS Institute Inc., Cary, NC, USA). Statistical significance was accepted at a p-value of <0.05.
RESULTS
The baseline characteristics of patients using intrawound vancomycin powder and the conventional method are summarized in Table 1. The mean age (p=0.001) of patients using intrawound vancomycin powder was higher than that of those using the conventional method. History of diabetes mellitus (p=0.007), non-smokers (p=0.016), and severe disability (modified Rankin scale score of 5, p=0.130) were more frequent, and preoperative C-reactive protein levels (p<0.001) were higher in patients using intrawound vancomycin powder. When choosing an artificial material for cranioplasty, titanium (p<0.001) was more preferred in patients using intrawound vancomycin powder. These six variables were included as covariates in outcome comparison.
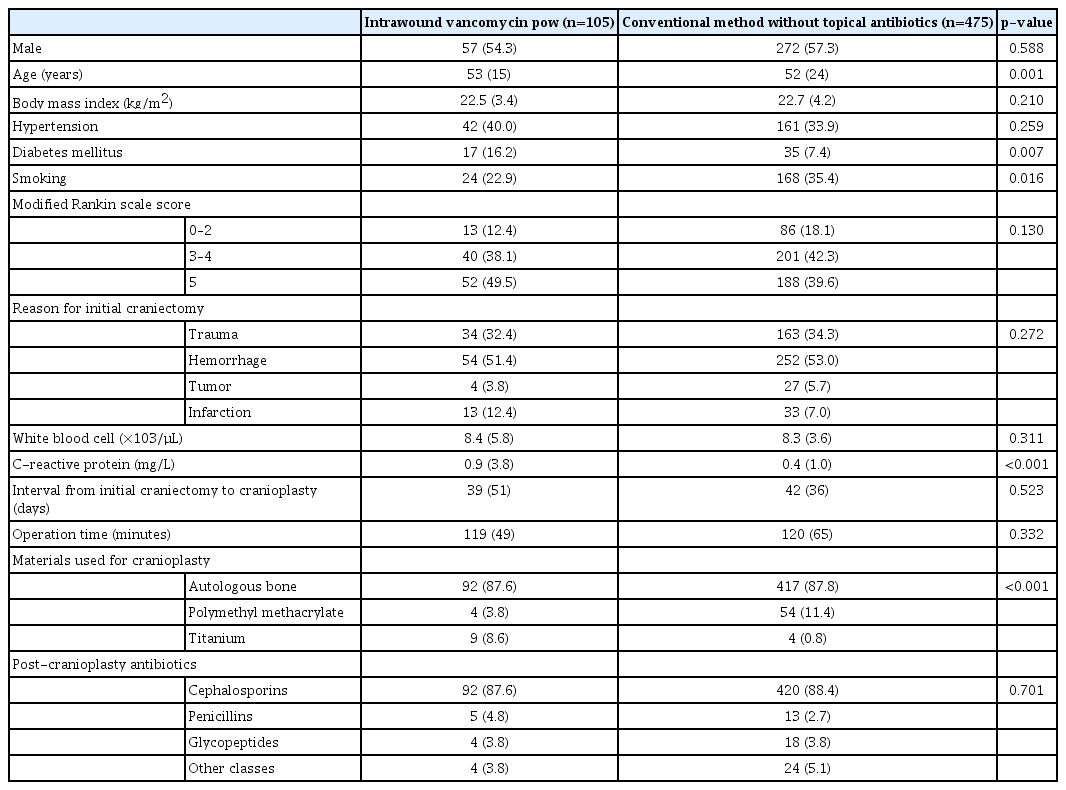
Baseline characteristics of patients receiving cranioplasty using intrawound vancomycin power and the conventional method without topical antibiotics
Surgical site infections following cranioplasty occurred in 31 patients (5.3%) (Table 2 and Supplementary Table 1). All were observed in patients who underwent cranioplasty using the conventional method. The median time between cranioplasty and the detection of surgical site infection was 13 days (range, 4–333). Staphylococci were the most common organisms. They were identified in 25 (80.6%) of 31 cases with surgical site infections. As a main treatment for surgical site infection, re-surgery was performed in 28 (90.3%; wound revision and only debridement of infected tissue in 10 [32.2%] and wound revision including bone f lap removal in 18 [58.1%]) and antibiotic therapy only was used in the remaining three cases (9.7%). Six patients (19.4%) underwent re-cranioplasty after surgical site infection control. However, surgical site infection recurred, and the bone flap was eventually removed in four patients (12.9%). On final follow-up, 15 patients (48.4%) had skull defects and two patients (6.4%) died during treatment for surgical site infections.
In patients who underwent cranioplasty using intrawound vancomycin powder, no surgical site infection was detected during the 1-year surveillance period. Therefore, the surgical site infection rate in patients using intrawound vancomycin powder was significantly lower than that in patients using the conventional method (0/105 [0.0%] vs. 31/475 [6.5%]; crude OR, 0.067; 95% CI, 0.006–0.762). This difference was also found to be significant even when adjusted for age, diabetes mellitus, smoking, modified Rankin scale scores, preoperative C-reactive protein levels, and materials used for cranioplasty (adjusted OR, 0.068; 95% CI, 0.006–0.731; p=0.026). No adverse events associated with intrawound vancomycin powder were observed during the follow-up.
DISCUSSION
In this study, we found that surgical site infections were not infrequent in patients who underwent cranioplasty using the conventional method and application of vancomycin powder within the wound prevented surgical site infections following cranioplasty. The use of topical vancomycin did not yield any local or systemic adverse events which have been reported in other surgical fields.
Most patients with surgical site infections in this study underwent reoperation and received additional antibiotic therapy for a long time to control surgical site infections. Other studies reported that bone flap removal was required in 66–100% of patients with surgical site infections [2,4,12,26]. Similarly, we had to remove the bone flap in 18 (64.2%) of 28 patients who underwent re-surgery for surgical site infections. Thereafter, second cranioplasty was tried, but a considerable number of patients experienced surgical site infection recurrence and were eventually left with a skull defect. The application of vancomycin powder in the wound was a simple process during cranioplasty and effectively prevented surgical site infections. Therefore, we recommend adding this simple process to cranioplasty procedure, based on the results of this study.
In a literature review, Staphylococci were found to be the most common causative organisms of surgical site infections, accounting for 48–70% of the isolated organisms [1,19,23,27,29]. Our study also showed that Staphylococci were isolated from most surgical site infections in culture studies. Additionally, 96% of the Staphylococci were found to be resistant to methicillin, which was consistent with the results of another study conducted in Korea [13]. Based on these findings, vancomycin can be the first-choice antibiotic if topical antibiotics are used in cranioplasty.
The patients in this study experienced no adverse events associated with the use of intrawound vancomycin, which is consistent with other published studies including cardiac and cranial surgeries [7,22,24,25]. However, several local (wound dehiscence, wound seroma, delayed wound healing, neuritis, and pseudoarthrosis) and systemic (anaphylactic reaction, renal toxicity, and ototoxicity) adverse events have been reported in spinal and orthopedic surgeries in which the effect and safety of intrawound vancomycin powder were most extensively evaluated [5,6,8,11,18,21]. Therefore, as recommended in these surgical fields, minimizing the amount of vancomycin powder and hemovac line placement for avoiding an over-concentration of vancomycin in the wound can be helpful for reducing adverse events. In our experience, 1 g of vancomycin powder was usually sufficient to cover the entire surface of the dura and bone flap before wound closure.
This study had several limitations. First, this was a retrospective cohort study. Thus, some confounding variables that could be associated with outcomes might have been missed and not included in the outcome comparison for effect adjustment. However, because the outcome difference between the two study groups is large, it is statistically impossible that our results are changed by effect of these missing variables. Second, the electrical medical record system in our institution has been changed several times. Therefore, some events, especially minor surgical site infections, could have been missed in the older medical records. Because cranioplasty was performed by the conventional method in all patients during the period in which older medical records were used, surgical site infections were more likely to have been missed in patients using the conventional method. Third, since the data used in this study were based on multi-surgeons’ experiences that differed in surgical techniques, this could have made a difference in the incidence of surgical site infections. Nevertheless, considering that the rate of surgical site infections decreased sharply after the application of intrawound vancomycin powder, we do not think that surgical techniques or experiences influenced key results of this study. Fourth, first-generation cephalosporin was administered intravenously for 7 days after cranioplasty. We disclose that this policy is not a general rule for surgical site infection prevention. Lastly, we used single-center data for this study. The environment which can affect surgical site infections is usually different in each hospital. Therefore, our results need to be confirmed with multi-center studies for generalization.
CONCLUSION
We found that intrawound vancomycin powder prevented surgical site infections following cranioplasty which led to reoperation and long-term antibiotic therapy, without local or systemic adverse events. Our results suggest that intrawound vancomycin powder is an effective and safe strategy for patients undergoing cranioplasty.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Informed consent
This type of study does not require informed consent.
Author contributions
Conceptualization : GH; Data curation : SBY, GH; Formal analysis : GH; Methodology : SBY, GH; Project administration : GH; Visualization : SBY, GH; Writing - original draft : SBY, GH; Writing - review & editing : SBY, GH, HGK, JSK, HCK, SHO, MKK, BSC, JKR, SHS
Data sharing
None
Preprint
None
Supplementary materials
The online-only data supplement is available with this article at https://doi.org/10.3340/jkns.2023.0024.
Detailed summary of 31 patients with surgical site infection

