Maoneo, Beltchika, Kabulo, and Ntsambi: Letter to the Editor : Extramedullary Intradural Calcified Meningiomas Surgery in Limited Resources Context
To the Editor,
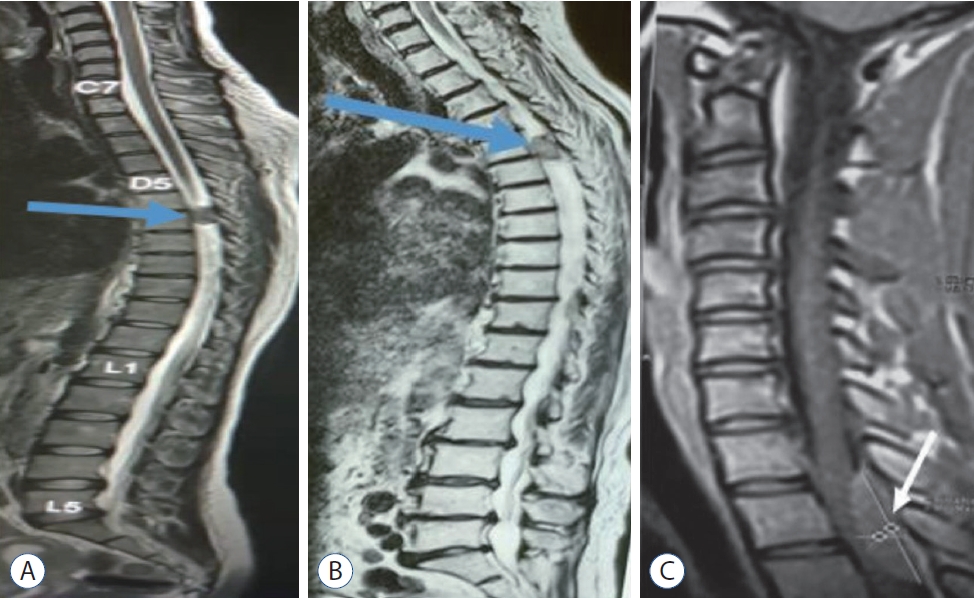
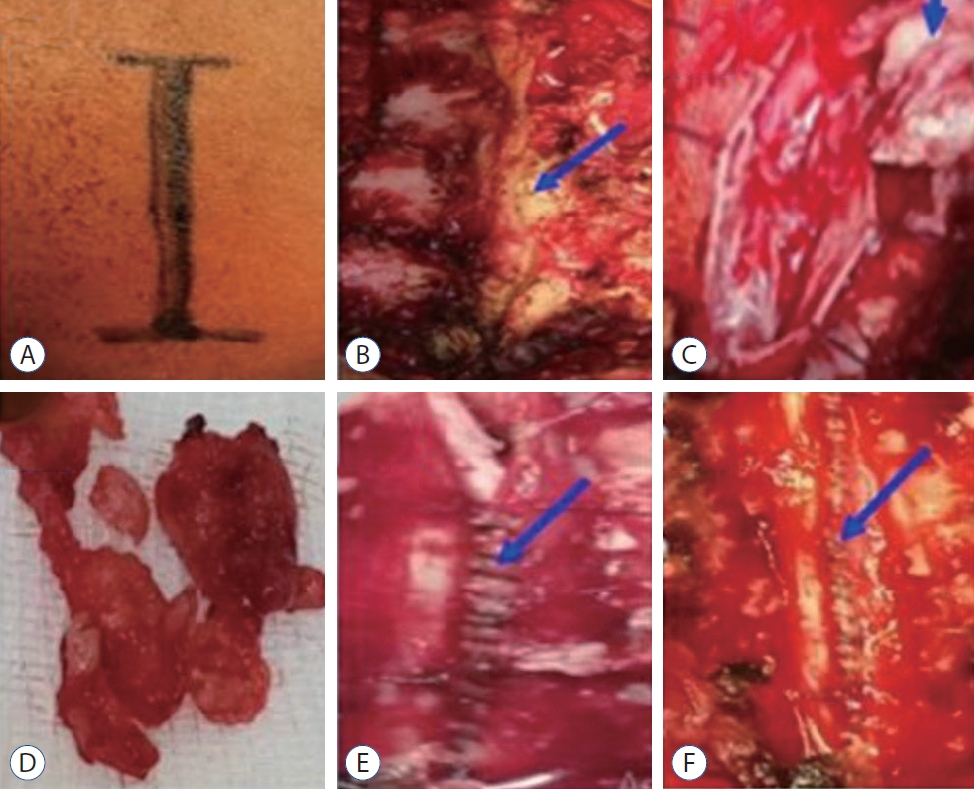
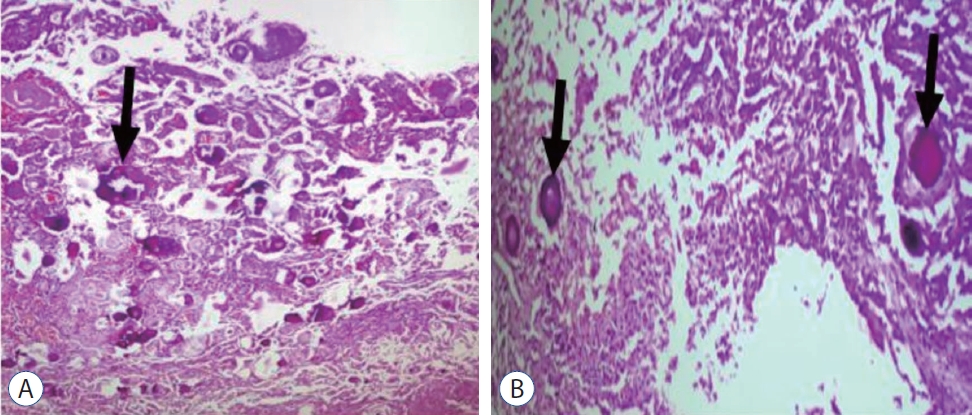
Spinal meningiomas are benign, slow-growing tumours, developed from arachnoidal cap cells [ 4]. Calcified forms are about 1-5% of all meningiomas [ 3]. Complete surgical removal of calcified spinal meningioma remains a true challenge in a context of limited resources without a neurosurgical microscope because of possible dural sac and nerve roots adhesions [ 3, 4]. We write this letter to the editor with the aim to explain our critical circumstances of the work according to three patients. We experienced three cases of calcified spinal meningiomas, the clinical features are summarized in Table 1. Fig. 1 shows the magnetic images taken before the operation. In all three cases, our surgical procedures consisted of ( Fig. 2) : 1) identification of the level using the MRI or CT-scan images. We performed laminectomy of two or three levels depending on the extent of the tumor on the imaging. 2) Complete release of the dural sac posteriorly and postero-laterally. 3) Instrumental palpation of the tumor mass to assess the consistency. 4) Then longitudinal durotomy of about 3-4 cm of the external dural layer using micro-instruments, going beyond the tumour region on either side. 5) Gradual dissection of the tumor by removing the adherent internal dural layer while meticulously separating the rootlets attached to the mass according to Saito et al. [ 6] techniques using micro-instruments. 6) After complete resection of the tumor, control of hemostasis using surgicel followed by watertight closure of the external dural layer using 3/0 vicryl with no use of biological glue. And 8) porto vac drain was left in situ then suture by layer. No dural defects were observed apart from the surgical opening. The specimen taken and sent for histology came back as psammomatous (calcified) meningioma ( Fig. 3). Calcified spinal meningiomas are frequently observed in women over 50 years old, located in the thoracic spine. However, they are also found in people under 50 years of age usually associated with a poor prognosis [ 2]. The signs can be confused with other diseases in elderly people and delay the diagnosis [ 1]. The delay in diagnosis is also due to the unavailability and accessibility of CT scan and MRI in countries with limited resources such as ours. Complete removal of the tumour, according to Simpson’s grades I, II, and III, is the best treatment for spinal meningioma. But the risk of cerebrospinal fluid leakage and recurrence is high [ 5]. The novel technique, similar to Simpson II, developed by Saito and colleagues [ 6] that consists of removing the meningioma with the inner layer of the dura and keeping the superficial layer for closure has got excellent results [ 7]. Many neurosurgeons use a surgical microscope during the operation. However, in a context of limited resources, this valuable tool is not always available. In the cases reported, we performed a macroscopically complete removal of the mass with the medial layer of the dura according to the procedure of Saito et al. [ 6] without neurosurgical microscope. These cases show the possibility of a complete recovery after a total macroscopic resection, even in a less elderly patient by using Saito technique without a neurosurgical microscope in limited resource context and the risk of the comorbidity in an elderly person.
Fig. 1.
Preoperative sagittal magnetic resonance images of case 1 (A), 2 (B) and 3 (C). T2 weighted image shows an intradural and extramedullary meningioma (blue arrow in A, B; white arrow in C). 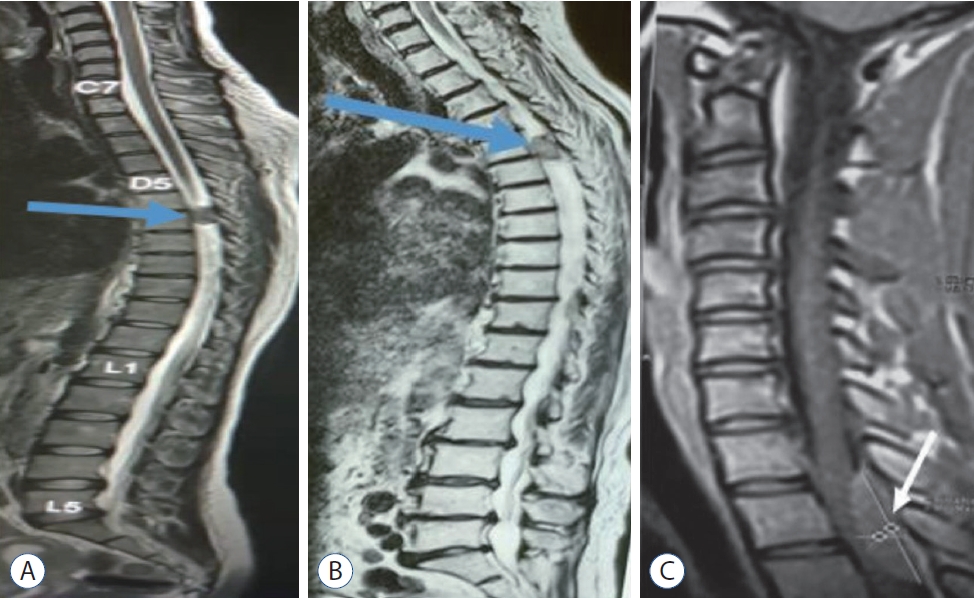
Fig. 2.
Intraoperative images showing. A : The posterior approach. B : The spinous processes resection and laminectomy (blue arrow). C : The dural opening through a longitudinal incision and the detachment and removal of the meningioma with the internal layer according to Saito et al.6). D : The meningioma mass resected. E and F : A watertight suture of the dural superficial sheet (blue arrow). 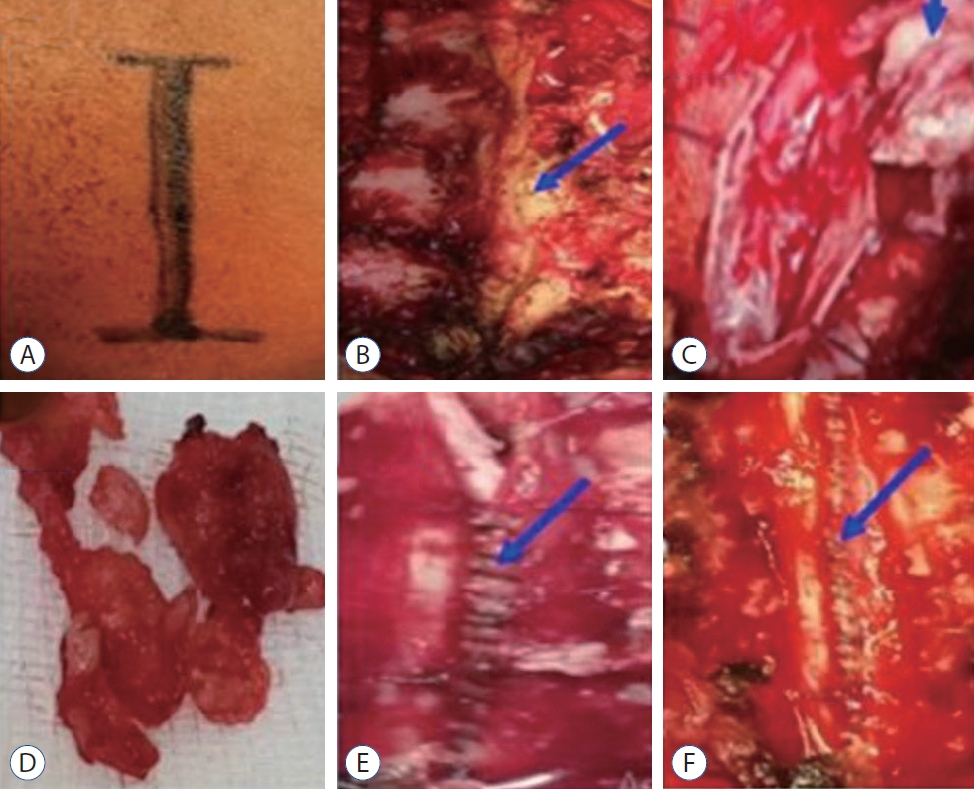
Fig. 3.
A and B: Histopathology picture shows numerous calcification foci (psammomas) (black arrow) (A : Hematoxylin and Eosin [H&E] staining, ×10; B : H&E staining, ×40). 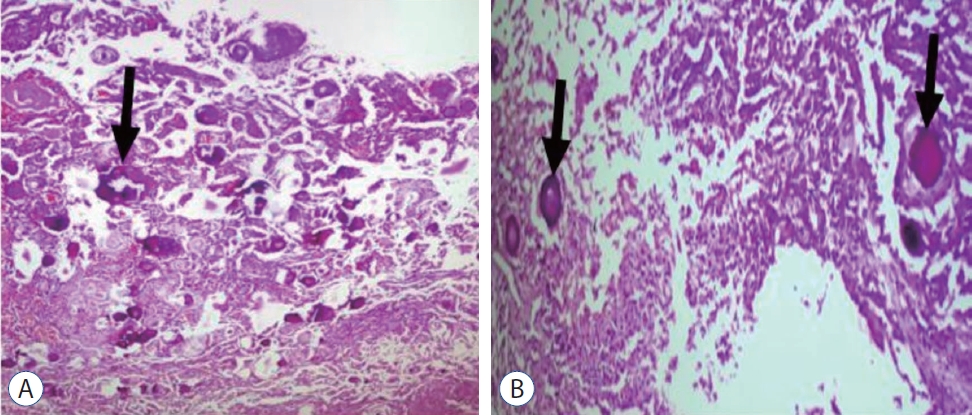
Table 1.
Clinical Summary of three patients
|
Case No. |
Age (years)/sex |
Location of tumor |
Neurological findings |
Treatment outcome |
|
1 |
29/F |
T7 |
Paraparesis, sensory deficit, hyperactive DTR |
Total removal, good recovery |
|
2 |
69/F |
T5, 6 |
Paraparesis |
Total removal, death due to medical problem |
|
3 |
20/F |
T2, 3 |
Paraparesis, sphincter change |
Total removal, good recovery |
References
1. Apostolov G, Kehayov I, Kitov B : Clinical aspects of spinal meningiomas: a review. Folia Med (Plovdiv) 63 : 24-29, 2021  2. Cohen-Gadol AA, Zikel OM, Koch CA, Scheithauer BW, Krauss WE : Spinal meningiomas in patients younger than 50 years of age: a 21-year experience. J Neurosurg 98( 3 Suppl):258-263, 2003   3. Kim JY, Min WK, Kim JE, Park KH, Mun JU : Two case reports of calcified spinal meningioma and a literature review. J Korean Soc Spine Surg 23 : 227-233, 2016   6. Saito T, Arizono T, Maeda T, Terada K, Iwamoto Y : A novel technique for surgical resection of spinal meningioma. Spine (Phila Pa 1976) 26 : 1805-1808, 2001  
|
|